A 51-year-old man presented with chronic right sub-costal pain and liver mass discovered by ultrasound. There were no significant findings on physical examination. He did not have any clinical features of chronic liver disease, including history, physical examination, and laboratory results. His viral hepatitis panels were unremarkable. His liver function tests were within normal limits, except for alkaline phosphatase at 154 IU/L (42-121), aspartate transaminase at 384 IU/L (12-32), and alanine aminotransferase at 170 IU/L (4-36). The carbohydrate antigen (CA19-9) level was at 33.1 (0-37) IU/L. He underwent computed tomography of the abdomen that revealed cystic lesions at the left hepatic duct, and magnetic resonance cholangiopancreatography revealed several side-by-side cysts with upstream dilatation of the adjacent bile duct (Fig. 1). Owing to the high prevalence of bile duct tumors, intraductal papillary neoplasms of the bile duct (IPNB), in our region, the patient was advised to have an endoscopic examination of the bile duct. Endoscopic retrograde cholangiopancreatography was performed to be a route for peroral cholangioscopy, but the procedure was unable to be performed due to a failure of cannulation into the common bile duct. Since the possibility of bile duct tumor was not fully eliminated, the patient therefore opted for a surgical resection rather than observation or re-endoscopic retrograde cholangio-pancreatography. During the left hepatectomy operation, intraoperative ultrasound was performed, revealing several side-by-side simple cystic lesions near the bile duct of segment 2 of the liver (Fig. 2a). After finishing the operation, we performed cholangioscopy of the surgical specimen, to evaluate the mucosa and status of bile duct communication, using a cholangioscope (Olympus; CHF type V: 4.9 mm). We found the normal mucosa of the biliary tract and external compression at the bile duct side wall without a bile duct communicated lesion (Fig. 2b, c). The surgical specimen revealed multiple varying-in-size simple cystic lesions lying near the bile duct segment 2 of the liver (Fig. 2d). The postoperative course was uneventful.
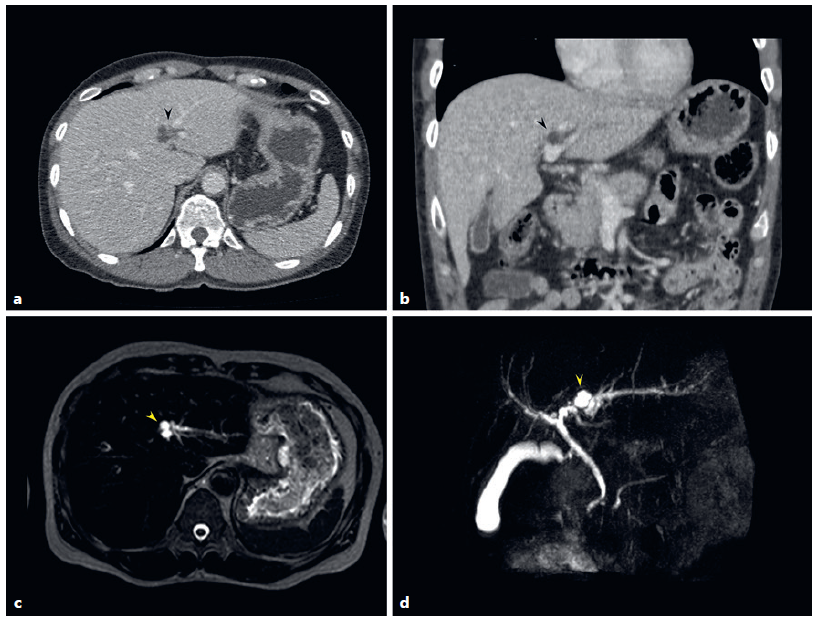
Fig. 1 Preoperative imaging of the patient. a, b CT scan revealed cystic lesions at LHD (black arrowhead). c, d MRCP revealed several side-by-side cystic lesions (yellow arrowhead) with upstream dilatation of the adjacent bile duct. CT, computed tomography; MRCP, magnetic resonance cholangiopancreatography.
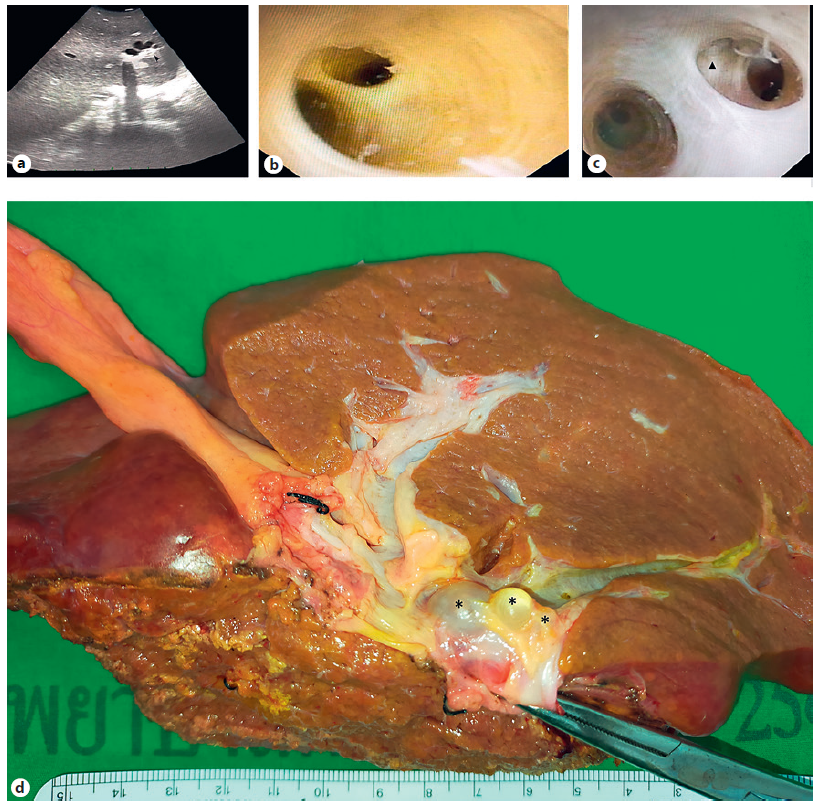
Fig. 2 Intraoperative findings. a IOUS showed several side-by-side simple cystic lesions near the bile duct of segment 2 of the liver. b, c Intraoperative choledochoscopy revealed normal mucosa of the biliary tract. The external compression was noted at the bile duct wall (triangle) without bile duct-lesion communication. d Surgical specimen revealed multiple varying-in-size simple cystic lesions (asterisk) lying near the bile duct of segment 2 of the liver. IOUS, intraoperative ultrasound.
Peribiliary cysts are one of the most recently de-scribed entities of liver lesions. These cysts are variable in size, with variable numbers coursing along the hepatic hilum and intrahepatic large bile duct, situated externally to the bile duct wall, and not communicating with the biliary lumen. The intrahepatic location is the most frequent type. Although these cysts are benign, they can frequently cause symptoms and occasionally cause biliary obstruction, leading to cholangitis [1]. Despite the presence of the typical features of diagnosis as a linear collection of numerous small simple cysts paralleling the portal and biliary structures (Fig. 3a, b), there have been a number of misdiagnoses and the occurrence of therapeutic misadventures [1]. Although peribiliary cysts have been extensively described by their unique radiologic findings, their real surgical specimens and cholangioscopic findings demonstrating pathoradiologic correlation are rarely to be found. The differential diagnosis of multicystic lesions of the liver ranges from benign lesions with no clinical significance to malignancies which are potentially lethal [2]. Hereafter, we compare the typical features of cross-sectional imaging of our patients, among the diseases with multiple-cystic-lesion appearances; these should be differentiated from peribiliary cysts, including polycystic liver disease, Von-Meyenberg complex, Caroli disease, and IPNB (Fig. 3c-j). The last one, IPNB, is also a notable mimicker of cystic liver lesion through unique progression and various morphologies [3].
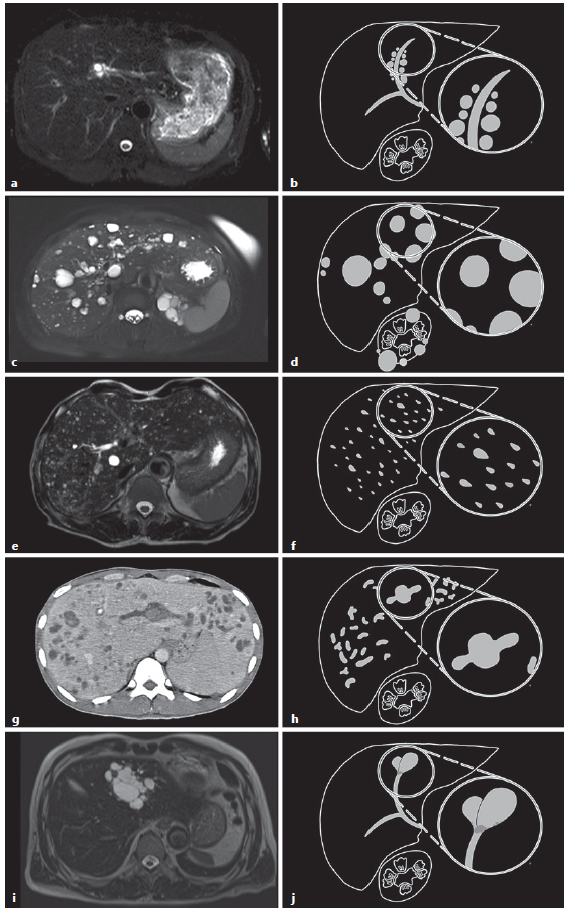
Fig. 3 Comparison of typical features of cross-sectional imaging (a, c, e, g, i) and illustrated diagram (b, d, f, h, j) among diseases with multiple-cystic-lesion appearance. a, b Peribiliary cysts; multiple small simple cysts alongside the bile duct without bile duct communication. c, d Polycystic liver disease; innumerable varying-in-size simple cysts scattered around the liver and often kidneys. e, f Von-Meyenberg complex (also known as biliary hamartomas); multiple small irregular varying-in-size cysts scattering around the liver. g, h Caroli disease; diffuse, mostly saccular, and fusiform dilatation of the intrahepatic bile duct, with a “central-dot” sign. i, j IPNB; localized marked cystic dilatation of the bile duct with usually identifiable intraluminal lesions














