Gastroparesis is a chronic disorder characterized by delayed gastric emptying without evidence of stomach or proximal small intestine obstruction [1]. Its pathophysiology is unclear, although gastric arrhythmias, fundal and antral hypocontractility, pylorospasm, and antropyloroduodenal incoordination might be involved [1]. Dietary modifications and prokinetics are first-line treatments. When refractory gastroparesis is present, surgical or endoscopic treatment must be considered.
We present a case of a 68-year-old female patient, followed in gastroenterology consult due to nausea, persistent postprandial vomiting, early satiety, and belching.
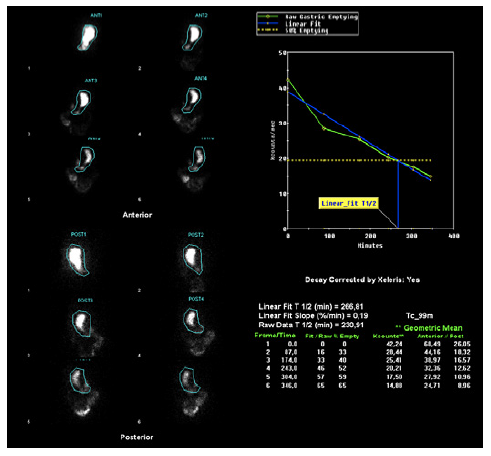
She has no relevant past medical or surgical history or medication. Esophagogastroduodenoscopy revealed food stasis but was otherwise normal. Gastric emptying scintigraphy (GES) showed emptying of 30% at 156 min, 46% at 217 min, and 54% at 260 min, with significant radiopharmaceutical retention (46% at 4 h 18 min), translating scintigraphic evidence of delayed gastric emptying (Fig. 1). The diagnosis of gastroparesis was made, and medical therapy was optimized. She had no improvement after 6 months, traducing a Gastroparesis Cardinal Symptom Index (GCSI) score of 3.33 points (0-5 points) [2]. Idiopathic refractory gastroparesis was admitted, and gastric peroral endoscopic myotomy (G-POEM) was proposed.
The procedure was performed with an endoscope (GIF-HQ190; Olympus Medical Systems, Tokyo, Japan), with a transparent distal cap (DH28GR; Fujifilm, Tokyo, Japan) and insufflation with CO2. The patient was under general anesthesia and orotracheal intubation. The VIO®3 (Erbe Elektromedizin GmbH, Tuebingen, Germany) was used as the electrosurgical unit. Antibiotic (cefotaxime 1 g) was administered. The procedure began with submucosal injection, in the greater gastric curvature, 5 cm proximal to the pylorus with a solution of 100 mL normal saline, 1 mL indigo carmine, and 1 mL adrenaline, followed by a mucosal longitudinal incision with a triangletip knife, using dry-cut current effect 2. Then, a submucosal tunnel was created from the mucosal incision to the pylorus, with spray-coagulation current. Full-thickness pyloromyotomy involving circular and oblique muscle bundles was performed, from the pylorus extending 3 cm proximally toward the antrum (using triangletip and IT-nanoTM knives [KD-640L, KD-612L/U; Olympus] with spray-coagulation and Endocut Q currents). The mucosal incision was closed with several clips (online suppl. video; see https://www.karger.com/doi/10.1159/000527016 for all online suppl. material,; Fig. 2a-f). The procedure was uneventful. On the day after, a gastroduodenal transit excluded leakage. She started a liquid diet, with good tolerance, and was discharged on the second day, medicated with 40 mg pantoprazole bid and ciprofloxacin for 7 days. She was on a soft diet for 1 week and then proceeded to small meals low in fiber and fat.
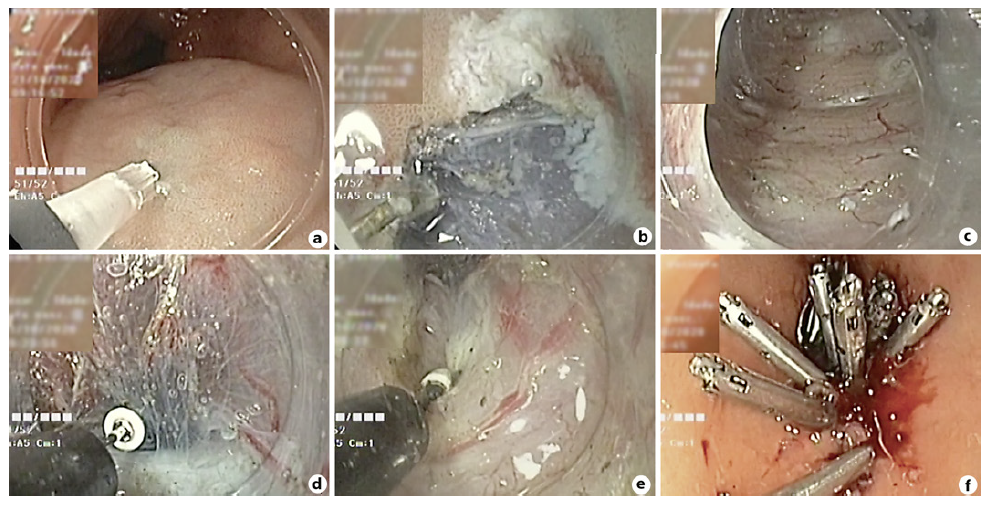
Fig. 2 a Submucosal injection 5 cm proximal to the pylorus. b Mucosal longitudinal incision. c Submucosal tunnel creation from the mucosal incision to the pylorus. d, e Full-thickness pyloromyotomy - from the pylorus extending 3 cm proximally toward the antrum. f Mucosal incision closed with clips.
Three months post-procedure, the GCSI score was of 2.11 points. Reassessment scintigraphy showed 29% gastric emptying at 50 min, 64% at 113 min, and 95% at 194 min, with no evidence of delayed gastric emptying at any time (Fig. 3).
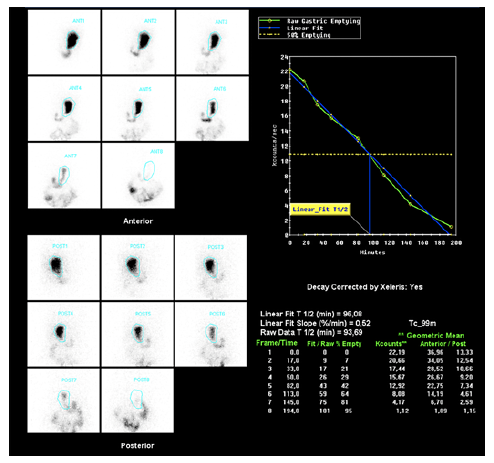
Fig. 3 Scintigraphic images after the G-POEM, with no evidence of delayed gastric emptying at any time.
G-POEM has a reported clinical success rate of 56-90% [3, 4], with described clinical improvement sustained up to 12-18 months after the procedure [3, 5]. Most adverse events are mild, being capnoperitoneum the most common [1, 3]. When compared to surgical pyloroplasty, G-POEM has similar clinical success in terms of GCSI score and GES, with comparable adverse events [1]. According to a multicentric prospective study, G-POEM should be considered in patients with more severe symptoms along with significant retention on GES [3]. The G-POEM represents an advance in the endoscopic approach of refractory gastroparesis, with the advantage of being a minimally invasive technique.