A 90-year-old woman, who underwent endoscopic ultrasound-guided hepaticogastrostomy for the B3 duct/segment by using a covered metal stent (CMS) (8 mm × 100 mm, Niti-S S-type stent; Taewoong Medical, Seoul, South Korea) 12 months earlier for extrahepatic bile duct cancer, was referred for the treatment of acute cholangitis. Food impaction into the CMS was found on endoscopy, and after the CMS removal, a 6-Fr nasobiliary drainage tube was then placed by hepaticogastrostomy. After 7 days of intravenous biapenem (0.3 g q12h), a novel antireflux CMS (10 mm × 60 mm, KAWASUMI Duck-bill Biliary Stent; Kawasumi Laboratories, Tokyo, Japan), which has a duckbill-shaped antireflux valve (DARV), was placed across the hepaticogastrostomy tract. However, the patient developed shaking chills and fever followed by hypotension 21 h after the CMS placement. Urgent endoscopy revealed that the DARV remained closed with pus coming out through the hepaticogastrostomy, which indicated acute obstructive suppurative cholangitis due to the DARV dysfunction (Fig. 1). After puncturing the DARV with a catheter to reduce the bile duct pressure, the stent was retrieved by a snare and was successfully replaced with a CMS without an antireflux valve (10 mm × 60 mm, X-Suit NIR fully covered; Olympus Medical Systems, Tokyo, Japan) (Fig. 2). No problem related to the CMS was observed until she died from the acute myocardial infarction 5 months later.
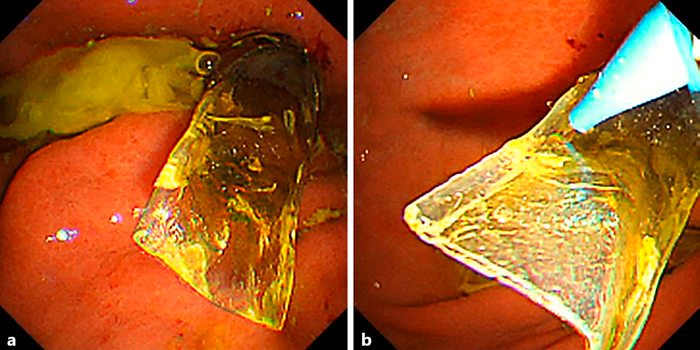
Fig. 1. Endoscopic images of an antireflux CMS placed across the hepaticogastrostomy tract showing pus coming out through the hepaticogastrostomy (a) and complete closure of the antireflux valve (b).
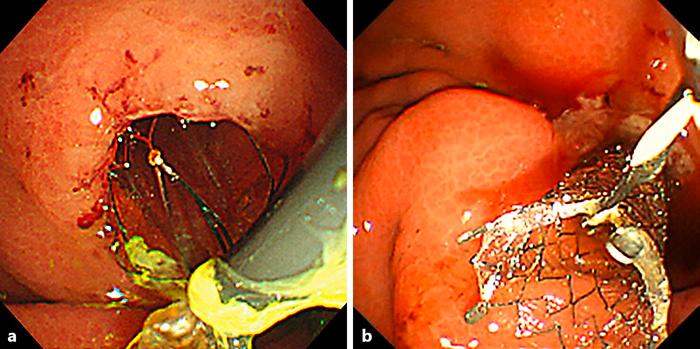
Fig. 2. Endoscopic images of hepaticogastrostomy stent replacement showing snare retrieval of an antireflux CMS (a) and a CMS without an antireflux valve placed across the hepaticogastrostomy tract (b).
Antireflux CMS has been developed to prevent the reflux of food or intestinal juice into the bile duct with the expectation of a longer time to recurrent biliary obstruction. To date, several types of antireflux valves have been applied to CMS: wineglass-shaped, nipple-shaped, long funnel-shaped, and windsock-shaped antireflux valve [1]. A meta-analysis of antireflux CMSs compared with conventional self-expandable metal stents concluded that antireflux CMS had a lower risk of stent occlusion [2]. In recent studies, CMS with DARV demonstrated a longer time to recurrent biliary obstruction than the conventional CMS [3, 4]. The DARV of the CMS is constituted by an expanded polytetrafluoroethylene membrane that extends beyond the distal end of the CMS. The DARV is usually closed to prevent the duodenobiliary reflux but opens when the bile duct pressure increases; however, in this case, even though the DARV was open when the CMS was deployed, the DARV remained closed as if sealed. Although to the best of our knowledge, antireflux CMS placement for other than distal malignant biliary obstruction has never been studied in much detail, the force of gravity may have prevented the biliary outflow from the DARV, and so clinicians should pay additional attention to the DARV dysfunction when placing the CMS with DARV across the hepaticogastrostomy.















