We present the case of a 79-year-old male with known history of sigmoid colon cancer, diagnosed in the context of bowel obstruction in 2018. In that setting, he was submitted to an emergent Hartmann procedure, maintaining the colostomy ever since. After staging (IIIB AJCC classification), the patient completed 6 months of adjuvant chemotherapy (CT). The first and last colonoscopy was 6 months after surgery. No relapse was noticed during the surveillance period. Three years later, he developed oropharyngeal dysphagia, without any other gastrointestinal symptoms. Physical examination showed an asymmetric tonsillar hypertrophy and multiple soft and painless cervical adenomegalies. He was referred to otorhinolaryngology and hematology at a cancer center. The tonsil biopsy showed a classic mantle cell lymphoma (MCL), and the chromosomal translocation t(11; 14) was identified by fluorescence in situ hybridization technique. The staging computerized tomography scan revealed adenopathies above and below the diaphragm, a large cecal mass (shown in Fig. 1c), and a heterogeneous appearance of the colic and ileal mucosa (shown in Fig. 1a, b). A total colonoscopy was performed, and, between the colostomy and the terminal ileum, multiple polyps were identified (shown in Fig. 2a-c and Fig. 2e), some of them with central umbilication. In addition, a vegetating mass measuring 55 mm in diameter was observed in the cecum (shown in Fig. 2d). Biopsies of the polyps in the ileum, ascending and descending colon, as well as cecal mass were performed, and, in all of them, pathology showed a monomorphic lymphoid cell infiltrate (shown in Fig. 3a). The lymphoid cells stained positive for CD20 and CD5 and negative for CD3 (shown in Fig. 3b). In addition, cyclin-D1 nuclear overexpression was observed (shown in Fig. 3c). The patient was diagnosed with an MCL stage IVA (Ann-Arbor classification), with a high-risk MIPIb score. After completing 2 cycles of R-bendamustine (rituximab and bendamustine), he was diagnosed with COVID-19, and CT was suspended. The MCL remained stable while waiting for virologic cure. The patient restarted CT with R-CVP (rituximab, cyclophosphamide, vincristine, prednisolone), and a reevaluation colonoscopy will be performed at the end of 6th CT cycle.
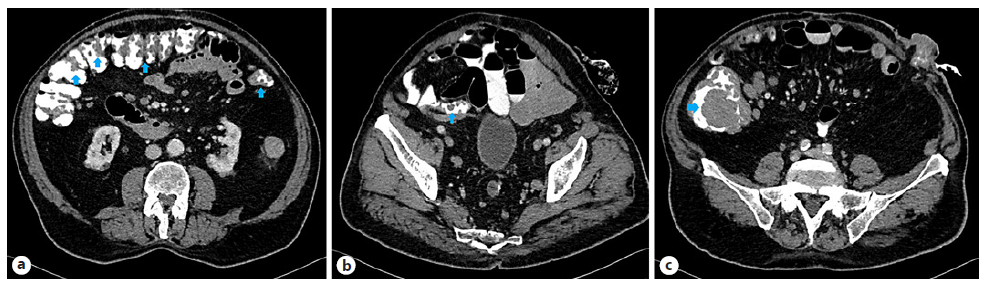
Fig. 1 Computerized tomography scan showing heterogeneous changes in colic mucosa (blue arrows) (a) and in terminal ileum (blue arrows) (b). c Cecal mass (blue arrows).
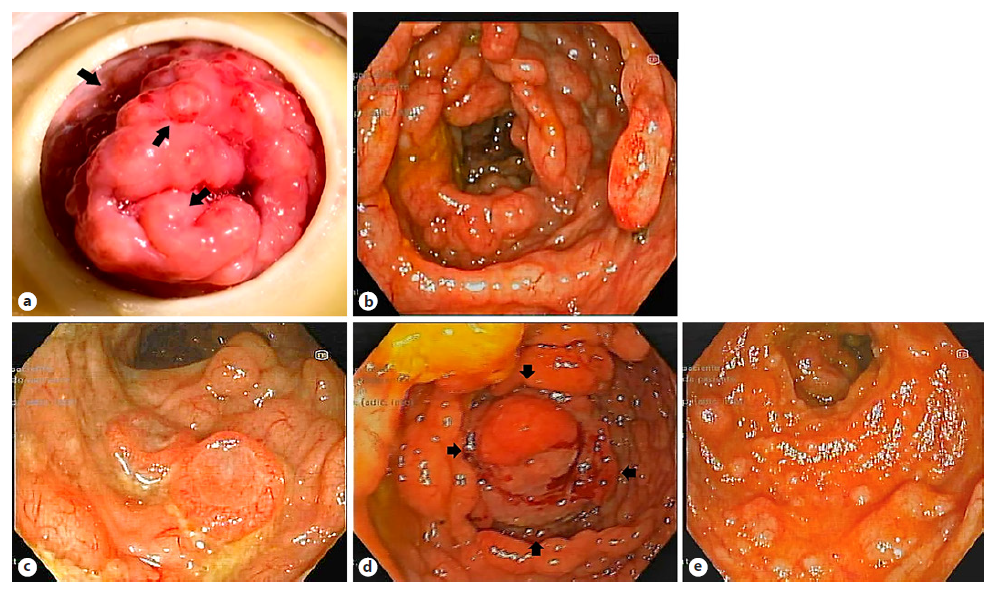
Fig. 2 Colonoscopy findings showing colostomy orifice with polyps on the surface (black arrows) (a); colon with multiple polyps (b); polyp with central umbilication (c); vegetating cecal mass - outlined by black arrows (d); terminal ileum with multiple polyps (e).
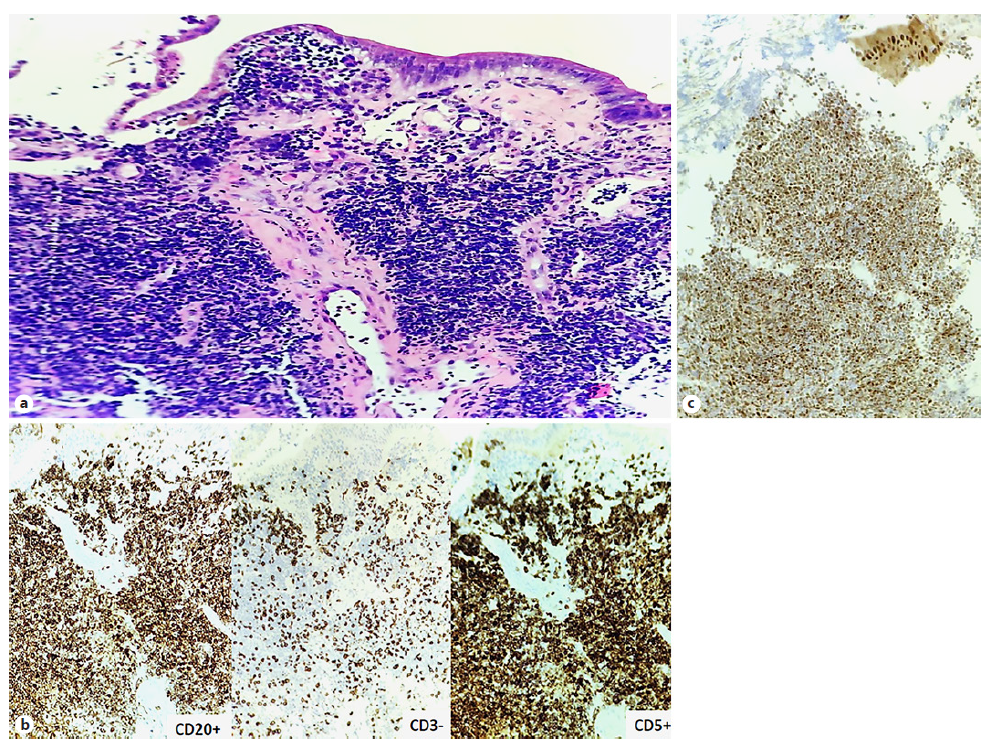
Fig. 3 Anatomopathological findings showing H&E ×100 showing a monomorphic lymphoid cells infiltrate (a); immunohistochemistry ×100 - staining positive for CD5 and CD20 and negative for CD3 (b); and overexpression of cyclin-D1 (×100) (c).
This case illustrates a silent presentation of an exuberant entity: multiple lymphomatous polyposis (MLP). MCL represents 6% of all non-Hodgkin lymphomas and is characterized by the chromosomal t(11; 14) which results in cyclin-D1 overexpression. The MCL affects mostly males in their 60-70 years and usually presents with disseminated disease, as seen in our patient [1]. Previously, gastrointestinal involvement was described in about 30% of the cases; however, it may be underestimated given the evidence of only microscopic involvement of the colon in about 84% of patients [2]. MLP is the most frequent colonic endoscopic finding of MCL, although isolated polyps or masses can also be found [3]. Besides lymphoma, the main differential diagnosis of MLP is intestinal pneumatosis. In younger patients, polyposis syndromes and inflammatory bowel disease should also be considered [4]. Regarding MCL treatment, the R-bendamustine regimen has the higher 5-year progression-free survival (65.5% vs. 55.8%), but the R-CVP regimen confers less immunosuppression [5].















