Gastric outlet obstruction (GOO) is a potential complication of gastric and pancreatic cancer, with additional morbidity and mortality [1]. Symptom relief is the main goal of interventional treatment, allowing resumption of oral diet, avoiding malnutrition and loss of quality of life. Endoscopic ultrasound-guided gastroenterostomy (EUS-GE) has emerged as an alternative to enteral stenting or surgery in this setting [2]. We present this single-center case series where EUS-GE was performed with technical and clinical success.
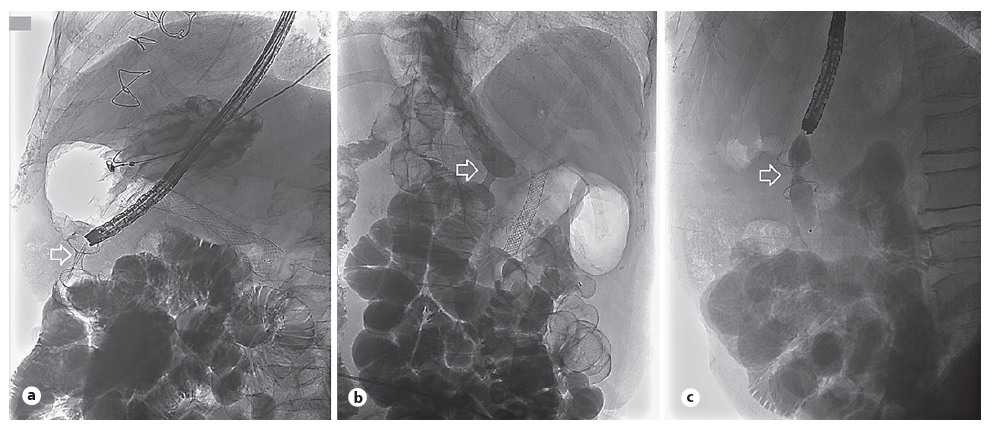
First, we describe the case of a 79-year-old male diagnosed with a metastatic poorly cohesive gastric carcinoma of the antrum, who refused chemotherapy. He developed food intolerance due to GOO, and a transpyloric uncovered self-expandable metal stent (SEMS; 22 mm × 9 cm; Evolution® Duodenal; Cook Medical, Bloomington, IN, USA) was initially placed with clinical improvement. After one month, symptoms recurred, and tumoral ingrowth of the SEMS was endoscopically confirmed. After a multidisciplinary team meeting, it was decided to propose the patient for EUS-GE. During the procedure, under general anesthesia with orotracheal intubation, 900 cc of saline solution with methylene blue was instilled, manually with syringe, to promote jejunal dilation, using a catheter (6 Fr × 200 cm, GLO-TIP II, Cook Medical, Bloomington, IN, USA), introduced through the stricture over a guidewire (0.035 in × 450 cm, JagwireTM; Boston Scientific, Marlborough, MA, USA). Under ultrasonographic guidance (Pentax EG38-J10UT linear echoendoscope; Pentax medical, Tokyo, Japan, with Hitachi-Aloka HI VISION Noblus processor), the bowel loop was accessed with a “wireless endoscopic simplified technique” (WEST), placing a Hot AXIOSTM lumenapposing stent (LAMS; 15 mm × 10 mm; Boston Scientific, Marlborough, MA, USA) through the lesser curvature of the stomach. The enteral communication was therefore created and then dilated with a through-the-scope balloon (Hercules® 3 Stage Wireguided; Cook Medical, Bloomington, IN, USA) up to 15 mm. Patient restarted oral food intake within 12 hours and remained food-tolerant until he deceased, 3 months after procedure.
Second, we present the case of a 75-year-old woman with a pancreatic ductal adenocarcinoma of the uncinate process, locally advanced with mesenteric vessels’ in-volvement, proposed only for palliative radiotherapy. She first presented with obstructive jaundice and underwent an endoscopic retrograde cholangiopancreatography with successful placement of biliary SEMS (6 cm × 10 mm, WallFlexTM Biliary RX Uncovered; Boston Scientific, Marlborough, MA, USA). Six weeks later, she developed GOO symptoms, and endoscopically, stricturing tumoral infiltration of the distal second portion of the duodenum was observed. After multidisciplinary team discussion, the patient was proposed for EUS-GE, which was performed with placement of a 20 mm × 10-mm LAMS through the posterior gastric wall using WEST. Balloon dilation was not performed because of mild self-limited bleeding. Liquid diet was resumed the day after and was successfully progressed with no limitations. The patient died 4 months after the procedure due to disease progression, with no GOO recurrence.
The last case describes a 58-year-old male with gastric adenocarcinoma of the antrum proposed for palliative chemotherapy and immunotherapy. One month after diagnosis, he developed nausea and early satiety complaints and, taking into account his good performance status, was proposed for EUS-GE. A 15 mm × 10-mm LAMS was placed through the posterior gastric wall, also using WEST, followed by stent balloon dilation. Eight months after the procedure, the patient is under transtuzumab with good clinical response and no GOO symptoms.
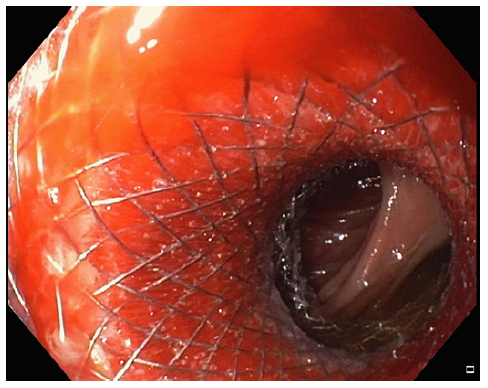
EUS-GE is reported to be an effective therapeutic alternative for GOO with rates of technical and clinical success around 90% [3, 4]. In this series, we used the WEST approach, allowed by the cautery-enabled LAMS single-step insertion that is believed to reduce stent misplace-ment chances (Fig. 1-3). Although there are now available balloon catheters that could help occluding a jejunal loop for puncture [4], successful bowel loop dilation was easily achieved by infusion through a regular catheter in all cases. EUS-GE allies the best and avoids the worst of both previous approaches, surgery and stenting, allowing minimal invasiveness, short time to oral refeeding, short hospital stay, and long-term patency, with low complication rates [5].
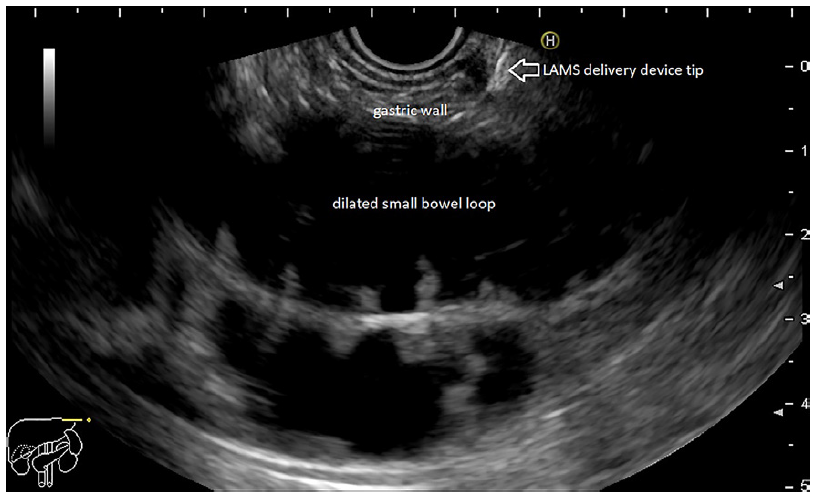
Fig. 1 Jejunal loop identified by EUS and preparation for direct puncture with the LAMS delivery system device - “freehand” technique.