Introduction
Malignant biliary distal obstructions usually present at late stages, precluding a curative therapeutic approach in most patients. The management of obstructive jaundice is of paramount importance, since it is associated with disabling symptoms, such as pruritus, and increased risk of cholangitis, hepatic disfunction, and liver failure. Undrained biliary obstruction is also associated with higher mortality, as shown by the series of Stark and Hines (2015), in which about 38% of patients with no palliative treatment died after complications of biliary obstruction [1, 2].
Historically, surgical biliodigestive anastomosis was the first method for biliary drainage in irresectable diseases, but it was associated with high rates of post-procedure mortality (rounding 15-30%) and up to 65% of morbidity [3]. Currently, endoscopic retrograde cholangio-pancreatography (ERCP) is the primary modality for biliary drainage, but it fails in up to 35% of cases. In patients in whom standard ERCP is not possible, percutaneous biliary drainage (PTBD) is a very effective procedure and represents an alternative to failed ERCP. However, it is associated with a rate of adverse events (AEs) ranging up to 33% of patients and also with increased morbidity and a negative impact in patient’s quality of life [4, 5].
Endoscopic ultrasound-guided biliary drainage, de-scribed for the first time by Giovannini and colleagues in 2001, has increasingly become an alternative method of biliary decompression, with high rates of technical and clinical efficacy, and fewer AEs than PTBD. Among the endoscopic ultrasonography-guided techniques, recent evidence has suggested that both EUS-guided choledo-choduodenostomy (EUS-CDS) and hepaticogastrostomy present high technical and clinical success rates, but EUS-CDS seems to be associated with short procedure times and less early AEs, possibly being a preferable method in the drainage of distal obstructions of the common bile duct (CBD) [6-9]. We aimed to evaluate the efficacy and safety of EUS-CDS performed in patients with distal malignant biliary obstructions, after failed ERCP.
Materials and Methods
Study Design and Patient Selection
We performed a single-center retrospective cohort study between July 2017 and June 2022 in a tertiary referral center for interventional endoscopy. We included all consecutive patients with malignant distal biliary obstruction (with malignancy confirmed/suspected by histology or radiologic studies) who failed ERCP-guided biliary drainage. We excluded patients under 18 years old, with malignant infiltration of the duodenal bulb and with CBD diameter inferior to 10 mm.
Procedure and Materials
All procedures were performed by an experienced endoscopist (LL) in ERCP (>300/year for the last 15 years) and EUS (>250 linear EUS/year for the last 10 years), with patients in left lateral position and under sedation with propofol, administered by an anesthesiologist. All EUS-CDS was performed with Pentax EG3870UTK (Pentax, Tokyo, Japan) or Olympus GF-UCT180 (Olympus, Tokyo, Japan) linear echoendoscopes.
Between 2017 and 2018, EUS biliary drainages were performed under fluoroscopy guidance, using fully covered biliary stents or lumen-apposing metal stents (LAMSs), according to the preference of the endoscopist and stent availability at the time of the procedure. The echoendoscope was advanced into the duodenal bulb, where the dilated CBD was identified. The CBD was punctured from the duodenal bulb using a 19-G needle (Expect, Boston Scientific), and a cholangiogram was performed. Subsequently, a 0.035-inch guidewire (JagwireTM, Boston Scientific) was introduced into the bile duct and the tract dilated with a 6-Fr cystotome (Cysto-Gastro-Set; EndoFlex, GmbH; endoCUT 40 W/effect 1). The stent was deployed using a fluoroscopy and endoscopy guidance. Since 2019, EUS-CDS was performed using a new electro-cautery-enhanced LAMS (HotAxiosTM ; Boston Scientific, Marlborough, MA, USA), under real-time ultrasound guidance using pure-cut electrocautery (100 W) to reach the CBD. The LAMS type (8 × 8 mm or 8 × 6 mm) was selected according to the endoscopist, and the proximal flange was released using an intra-channel technique. Figure 1 presents the technique of EUS-CDS.
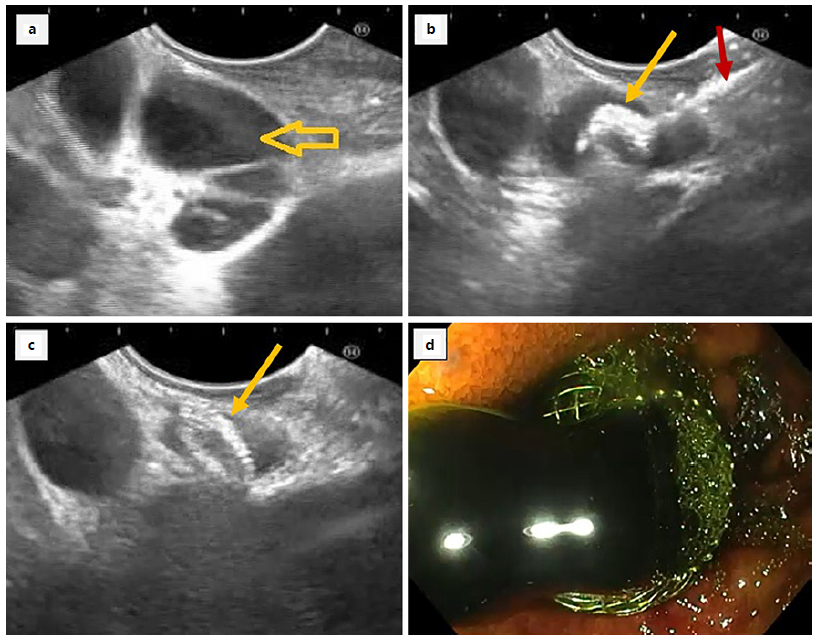
Fig. 1 Technique of endoscopic ultrasound-guided choledochoduodenostomy (EUS-CDS). a Ecoendoscopy showing a dilated common bile duct (yellow arrow). b HotAxiosTM distal flange placement in common bile duct lumen (yellow arrow) by an electrocautery-assisted device system (red arrow). c HotAxiosTM biliary stent opened and placed in common bile duct. d HotAxiosTM showing bile flow (duodenal perspective).
Outcome Measures
The primary outcomes were “technical success,” defined as “correct deployment of the stent between the CBD and the duodenum, with visualization of bile flow” and “clinical success,” defined as “resolution of jaundice or improvement in total serum bilirubin level above 50% at 7th day and above 75% at 30th day after the procedure.” Secondary outcomes were (i) procedure-related AEs, (ii) endoscopic reintervention, and (iii) survival time. AEs were defined as “early” if occurred within 30 days after the procedure or as “late” if after 30 days; we used the American Society for Gastro-intestinal Endoscopy lexicon to classify AE severity as mild, moderate, severe, or fatal [10].
Statistical Analysis
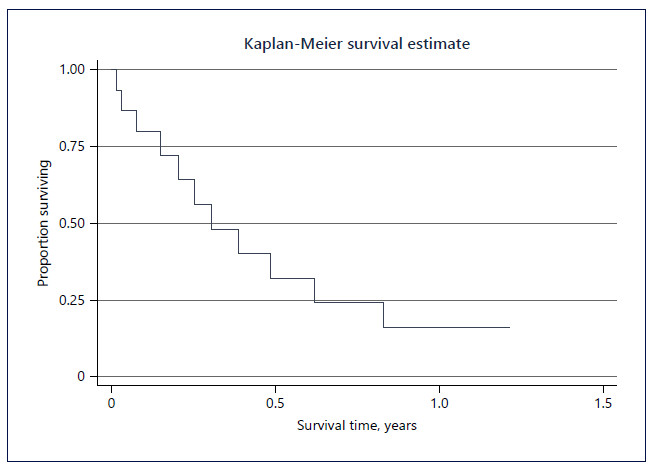
Continuous variables were described using the median and interquartile range; categorical variables were described as proportions and frequency counts. Overall median survival time was calculated from the time of the procedure until the patient’s death, and the Kaplan-Meier method was used for the survival analysis. Statistical Package of the Social Sciences® software (IBM SPSS Statistics for Windows, version 28.0.1.1) was used for data analysis.
Results
Patient’s Demographics and Clinical Characteristics
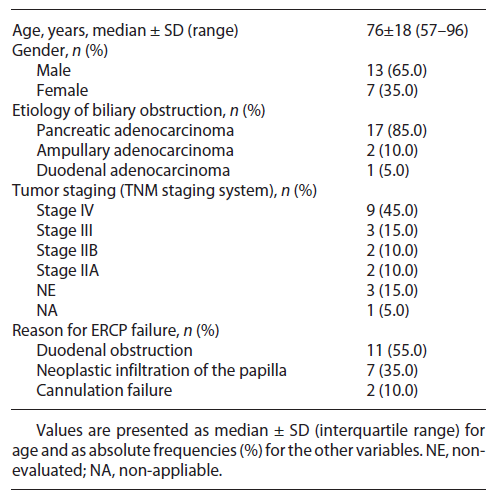
EUS-CDS was attempted in 20 patients (65.0% male), aged from 57 to 96 years old (median age 76 years) with malignant distal biliary obstruction, after failed ERCP. The most frequent etiology of the obstruction was pancreatic adenocarcinoma (n = 17; 85.0%), and most patients presented at late stages of cancer (60% in stages III or IV). In the majority of patients, failure of ERCP was secondary to a duodenal obstruction that precludes the passage of the duodenoscope into the second portion of the duodenum (n = 11; 55.0%). The patients’ demographics and clinical characteristics are summarized in Table 1.
Procedure-Related Outcomes
In 12 patients (60.0%), the EUS-CDS was performed in the same endoscopic session, immediately after ERCP failure. The remaining 8 patients (40.0%) were admitted from other hospitals, in which there were no available technical resources and/or experienced endoscopists in EUS-guided biliary drainage.
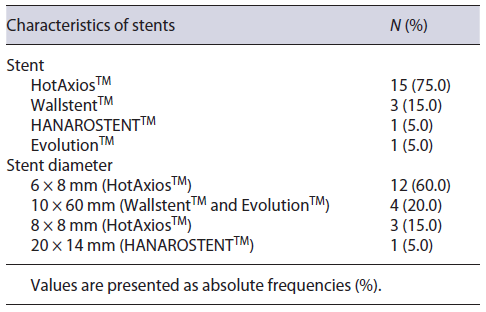
The obstruction resulted on a CBD median dilation of 14.5 mm (±5.5), ranging from 10 to 22 mm. HotAxiosTM was the chosen LAMS in all the 15 patients (75.0%) submitted to the procedure after the year 2019. The characteristics of stents are detailed in Table 2.
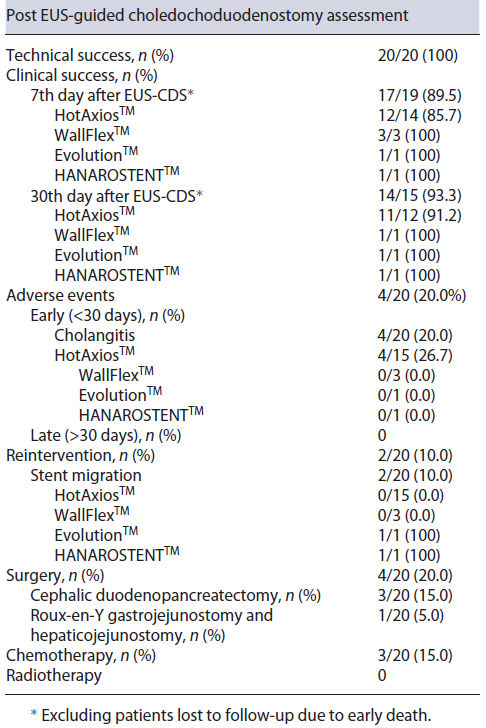
The stent was correctly placed in all patients (20/20), resulting in a technical success of 100%. Clinical success was achieved in 17 of 19 (89.5%) patients at the 7th day (1 patient died within the first week due to nosocomial pneumonia). At the 30th day, the clinical success was 93.3% (14/15); during this time, 4 patients have died: 2 patients in the sequence of nosocomial pneumonia and 1 patient, in whom palliative Roux-en-Y gastrojejunostomy and hepaticojejunostomy were performed, died after fecaloid peritonitis in the context of surgical anastomosis dehiscence, and the fourth patient died due to general condition deterioration (evolution of primary disease). Total serum bilirubin variation is shown in Figure 2.
Adverse Events
Four patients (20.0%) presented with cholangitis within the first 30 days after the procedure, in one case evolving into septic shock. All cases were medically managed with antibiotics and neither resulted in death. Other major complications, such as hemorrhage, perforation, peritonitis, or pancreatitis, were not observed.
Endoscopic Reintervention
In 2 patients (10.0%), a second endoscopic procedure was necessary, due to asymptomatic stent migration. In 1 case, the stent migration (EvolutionTM) to the gastric antrum was observed in an upper endoscopy performed for upper gastrointestinal bleeding, 9 months after the EUS-CDS. In the other case, an abdominal computed tomography performed 11 days after the procedure revealed HANAROSTENTTM migration into the proximal jejunum. Both cases occurred before the introduction of HotAxiosTM LAMS and were successfully managed endoscopically. Table 3 demonstrates the outcomes after the EUS-CDS procedure.
Follow-Up
The patients were followed for a median time of 93 days (±175), ranging from 5 to 751 days. In this time, 16 patients (80.0%) died because of disease-related complications.
Four patients (20%) were submitted to surgery: in 3 (15%), a cephalic duodenopancreatectomy was performed, with curative intent; in the remainder, a Roux-en-Y gastrojejunostomy and hepaticojejunostomy were performed due to irresectability of the cancer, observed during the surgery. Three (15%) patients received chemotherapy. Kaplan-Meier curve showing patient survival estimate after EUS-CDS is shown in Figure 3.
Conclusion
Our study represents the largest cohort of patients submitted to EUS-CDS in a Portuguese center and revealed that it is an effective technique for biliary drainage in patients with malignant distal biliary obstruction who failed ERCP, with a favorable safety profile when performed in an experienced center for advanced biliopancreatic endoscopy. To our knowledge, this is the first retrospective study to report the experience of EUS-CDS in a Portuguese population with malignant distal biliary obstruction.
Currently, ERCP is the first-line strategy in the drainage of malignant biliary obstructions but even when performed by experts, it is not successful in up to 35% of patients, due to stomach or duodenal obstruction, surgicalaltered anatomy or to anatomic changes of the papilla that prevent its cannulation. In our cohort, all patients submitted to EUS-CDS presented with duodenal obstruction, malignant infiltration of the papillary area, or an intradiverticular papilla that precluded successful ERCP. Although some recent studies suggest the repositioning of EUS-CDS as the initial choice for biliary drainage, in our department we use ERCP, reserving EUS-CDS for failed cases, as recommended by major endoscopy societies and reported from a large number of tertiary centers [4, 9].
EUS-CDS has emerged as an alternative to PTBD in cases of impossibility or failure of biliary drainage by ERCP. Since its introduction, important technical upgrades were observed, particularly with the emergence of the LAMS, the development of smaller stents - 6 and 8 mm - suitable for biliary drainage and, more recently, the addition of the electrocautery tip that allows direct fistulotomy within the bile duct, avoiding guidewire manipulation and biliary tract dilation [11].
Our results demonstrate that EUS-CDS was successfully achieved in all the patients, even though our patient’s median CBD size (14.5 mm) could be a risk factor for technical failure, as mentioned by Garcia-Sumalla et al. [12] who described that a CBD diameter above 15 mm was associated with higher technical success rates. Other studies also verified high rates of feasibility of EUS-CDS: for example, in the systematic review performed by Peng et al. [13] the pooled rate of technical success was 95.1% (CI = 90.6-97.5%; I2 = 255), while in another systematic review that only included studies published between 2015 and 2020, technical success rates ranged from 88.0 to 100%. Our high technical success may be in part explained by the utilization of the latest technical innovations in EUS-guided biliary drainage, as the electrocautery-enhanced delivery system allows a single-stage access and stent introduction, minimizing the procedure complexity. Besides, fully covered metal stents were used in all patients and these have demonstrated not only higher efficacy and safety but also an increased durability and patency rate, when compared to plastic and partially covered metal stents. Since 2019, HotAxiosTM was used in all patients submitted to EUS-CDS in our center; the rationale for this choice is the easiness of its insertion due to the cautery on the tip, as well as the presence of bilateral flanges that allow a better lumen-to-lumen apposition, with a reduced probability of stent displacement and biliary leakage [12-16].
For the analysis of clinical success, we excluded patients lost to follow-up due to early death, as none of the patients had died as a result of the procedure, but due to infectious or post-surgical complications or general status deterioration, so that the clinical success of the endoscopic technique cannot be affected by these losses. In fact, in 4 of the 5 patients who died before 30 days of follow-up, a greater than 50% decrease in baseline bilirubinemia was observed at some point. Our high clinical success - 89.5% at 7th day and 93.3% at 30th day after the procedure - is similar to previous studies: a recent sys-tematic review found a pooled clinical success rate of 93.3% (CI = 90.6-97.5%), and clinical success rates tend to be even higher in more recent systematic reviews, as the one performed by Ogura and Itoi, that reviewed EUS-CDS performances between 2015 and 2020 and found an overall clinical success rate of 97.0%, correlating this improvement with the new technical developments, like the ones we used in our patients [13, 15, 16].
The AE rate in our study was 20.0%, which is in line with previous published evidence on EUS-BD, that reported AE in 17-23% of patients. Over the years, it has been verified a changing trend in the EUS-guided biliary drainage AE rate: in their study, Ogura and Itoi subcategorized the analysis of EUS-CDS performance in 2 time periods and found that until 2015, the overall AE was about 16%, whereas since 2015-2020, there has been a slight improvement to about 12% of AE, possibly assignable to the experience and progression on the learning curve and, mostly, to the use of LAMS. In the same review, it was also verified a changing trend on the predominant complications: until 2015, the two most frequent AEs associated with EUS-CDS were perforation and bile leakage, but after 2015, cholecystitis and cholangitis predominate. The decreased utilization of plastic stents seems to justify these findings since they require previous dilation of the fistulous path, which is associated with higher bile leakage. On the other hand, self-expandable LAMSs seal the gap between the neofistula and the stent, preventing bile leakage and, therefore, biliary peritonitis. Another recent systematic review supports this, having found that self-expandable LAMSs were associated with significantly lower AE compared to plastic stents (17.52% vs. 31.03%; p = 0.013). Our study seems to accompany this trend, since cholangitis was the only major AE registered. Besides, all stent dysfunctions occurred before the beginning of HotAxiosTM utilization in our center, whose de-sign confers more stable CBD-duodenum anchorage. It is still unclear whether the insertion of a double-pigtail plastic stent through the LAMS improves the stent patency - the ongoing BAMPI trial will determine whether this technical variant offers a clinical benefit in EUS-CDS for the management of distal malignant biliary obstruction [15-19].
Although cholangitis was the only complication of EUS-CDS verified in our cohort, other relevant AEs are described in the literature. Of note, the most common intraprocedural complication of EUS-CDS using LAMS is stent maldeployment (particularly when the diameter of CDB inferior to 15 mm), and it can be managed by pre-loading a guidewire in the delivery system to guide the bile duct access after removing the misdeployed stent. In a long-term perspective, stent occlusion is the most frequent AE, with a median time of occurrence of 5-12 months [9, 20].
Although usually presented as a palliative procedure, 3 of our patients were submitted to surgery with curative intent and the presence of the stent (HotAxiosTM in all cases) did not prevent the performance of surgery. For years, the most used alternative to ERCP was PTBD. In their systematic review, Khashab et al. [21] found that compared to EUS-CDS, PTBD presents with similar technical success but slightly less clinical success. However, they verified that PTBD was associated with higher complications and need of reintervention, ultimately making EUS-CDS more cost-effective. Another recent systematic review concluded that when available, EUS-CDS may be preferable to PTBD due to a better safety profile, clinical and technical success. Based on current evidence, the European Society of Gastrointestinal Endoscopy strongly recommends that, when locally available, EUS-guided biliary drainage is preferred over PTBD, after failed ERCP, in malignant distal biliary obstruction [9, 21, 22].
As previously mentioned, several recent studies had concluded that EUS-CDS may be equivalent to ERCP as a primary method for the drainage of distal malignant biliary obstructions, showing comparable technical and clinical success rates. However, EUS-CDS has revealed both a reduced procedural time and a better safety profile, in particular in regard to the risk of postprocedural pancreatitis, that is null in EUS-CDS, since it is performed away from the major papilla [23].
Our study has some limitations, including the retrospective design and the absence of a control group (for example, of patients in whom PTBD was performed). Although the number of patients is not large, the sample size is not much inferior to most single-center studies from tertiary centers; to our knowledge, the single-center study with highest number of patients is the one of Matsumoto et al. [20] that included 151 participants; however, the patients were enrolled throughout a 14-year period, in a mean of 10 procedures per year, which reveals the relatively low number of EUS-CDS performed. With this in mind, there is the need of collecting data from a large number of centers in order to achieve meaningful insights as a randomized controlled trial with enough power faces huge challenges to be implemented.
Concluding, in our study EUS-CDS was an effective technique for biliary decompression in patients who failed ERCP. Further work is needed, including randomized and cost-effectiveness studies, comparing EUS-CDS with ERCP, to establish EUS-CDS as a primary drainage technique.