A 28-year-old female from Guinea-Bissau living in Portugal for 6 years presented with a 2-week history of intense epigastric pain with postprandial worsening, which was relieved by self-induced vomiting. Her past medical history was unremarkable. Laboratory investigation revealed eosinophilia (1.04 × 109/L; normal: 0.02-0.5 × 109/L; 15.5%, normal: 0-6%), without anemia (Hb 13.2 g/dL, normal; 12-15 g/dL; MCV 80 fL, normal: 80-96.1 fL) or raised CRP (0.17 mg/dL, normal: 0-0.5 mg/dL).
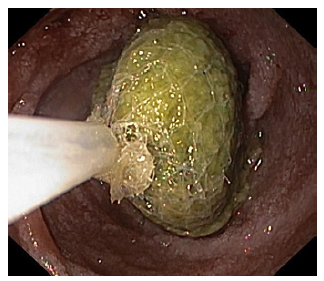
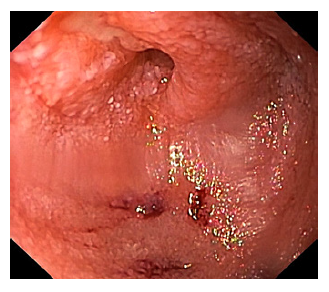
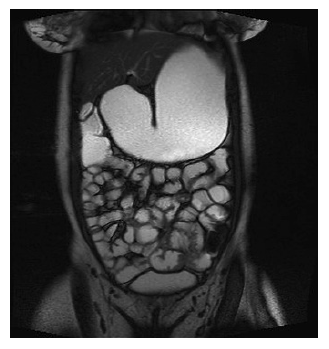
Esophagogastroduodenoscopy was performed, showing gastric dilation with food residue, an easily traversable circumferential narrowing at the duodenal bulb, and a small phytobezoar in the second duodenal portion (Fig. 1). Upon its removal, a linear ulcer was found which extended to the third duodenal portion, ending in a pinhole ulcerated stricture (Fig. 2). Biopsies were taken for histopathological, microbiological, and mycobacterial analysis. She underwent enteral-MRI, revealing a circumferential narrowing of the third portion of the duodenum (Fig. 3).
Fecal calprotectin was normal (46 mg/kg; normal: <80 mg/kg). Duodenal mucosa’s direct and cultural exams for mycobacteria were negative.
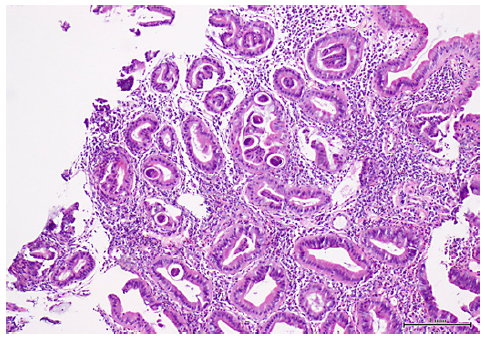
Histopathology showed expansion of the lamina propria at the expense of a mixed inflammatory infiltrate with eosinophils, as well as eggs and larvae of Strongyloides stercoralis (Fig. 4). Stool examination also revealed this finding. The diagnosis of duodenal obstruction due to S. stercoralis infectious duodenitis was made.
HIV infection was later excluded. The patient was treated with ivermectin 2 mg/kg for 2 consecutive days. Clinical, laboratory, and stool revaluation were scheduled at 1-month follow-up. On revaluation, she was asymptomatic, laboratory analysis showed normalization of eosinophils, and parasitological stool examination was negative. Due to loss of follow-up, endoscopic reassessment was not performed.
S. stercoralis is a parasitic nematode that infects the gastrointestinal tract through skin contact with contaminated soil [1]. It is more prevalent in tropical and sub-tropical regions [1]. It has the ability of completing its life cycle entirely within the human host to establish an auto-infection cycle.
Chronic infection by S. stercoralis is often asymptomatic and clinical manifestations can occur long after initial infection, including nonspecific gastrointestinal, dermatological, and respiratory symptoms [2]. Small bowel obstruction is a poorly recognized and probably underreported complication of S. stercoralis infection, with only a few cases reported in the literature [1]. Severe mucosal edema is suggested to be the cause of bowel obstruction in these cases [1].
Laboratory tools for diagnosis of strongyloidiasis include stool testing and serology. Due to the intermittent shedding of larvae, stool examination has a low sensitivity (<50%) [3]. Serologic testing using ELISA is nowadays the gold standard, presenting high sensitivity (89%) and specificity (97%) [4].
The prognosis of duodenal obstruction due to S. stercoralis infection is not well established. Nevertheless, late diagnosis seems to add to its dismal prognosis, mostly due to bacterial translocation and sepsis [1].
We herein present a case of strongyloidiasis in an immunocompetent patient who had been in a non-endemic area for years and whose only clinical manifestation was epigastric pain. The key point is that strongyloidiasis should be considered in the differential diagnosis of gastrointestinal symptoms, especially in patients from endemic areas, because diagnosis may be challenging, and immunosuppression can have dire consequences by inducing hyperinfection [2].