Endoscopic ultrasound biliary drainage (EUS-BD) has been increasingly used in the management of malignant biliary obstruction together with endoscopic retrograde cholangiopancreatography (ERCP). Drainage of ≥50% of hepatic volume is associated with an increase in survival and lesser risk of cholangitis, and bilateral drainage in hilar stenosis results in fewer reinterventions [1, 2]. When the left biliary system is drained through the papilla, EUS-guided hepaticoduodenostomy (EUS-HDS) is a difficult procedure that can be used to access the right system [3]. Combination of EUS-BD and ERCP (CERES) is in increasing development, particularly when the left and right biliary systems are non communicating [3, 4]. The authors present a case of EUS-HDS in the right hepatic duct combined with left hepatic duct stenting by ERCP in malignant hilar biliary obstruction (Fig. 1; online suppl. video; for all online suppl. material, see ).
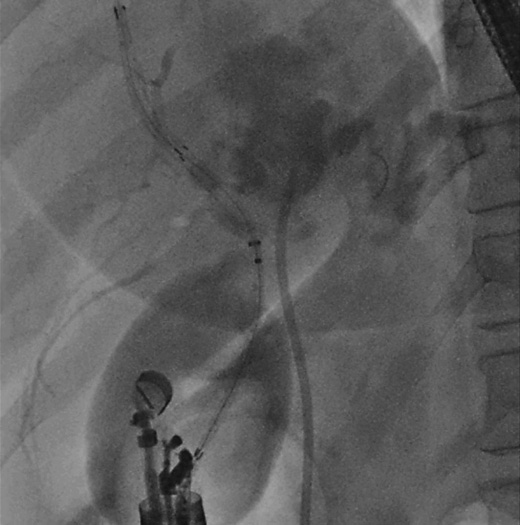
Fig. 1 Combined EUS-BD and endoscopic retrograde cholangiopancreatography in a malignant hilar biliary obstruction, restenting the left hepatic duct and hepaticoduodenostomy on the right hepatic duct, achieving bilateral drainage. EUS: after guidewire introduction, a hybrid metallic stent was placed between the right hepatic duct and the duodenal bulb.
A 60-year-old female patient with unresectable cholangiocarcinoma and hilar stricture (Bismuth type IV), with previous drainage of a technically difficult stricture of the left hepatic duct with a plastic stent, developed obstructive jaundice due to disease progression, incompatible with palliative chemotherapy. An ERCP was performed with plastic stent replacement in the left hepatic duct (Fig. 2a). Righ the patic duct stenting was not possible due to impossibility of passing a guidewire; cholangioscopy assistance was assumed to provide no further benefit because we were facing a very tight stricture, so EUS-BD was performed. EUS showed a dilated right hepatic duct (7.4 mm)(Fig. 2b). The right hepatic duct was punctured (Expect™ 19 G, Boston Scientific, Boston, USA), with confirmation by cholangiography (Fig. 3a). After guidewire introduction through the puncture site (Jagwire™ 0.0025″,Boston Scientific, Boston, USA), the needle was retrieved and a hybrid metallic stent (BPD HANAROSTENT® biliary [NC], 10*80 mm, M.I.Tech, Pyeongtaek-si, Gyeonggido, Republic of Korea) was placed between the right hepatic duct and the duodenal bulb (Fig. 3b, c). The stent delivery system was passed through the puncture site without the need of using a cautery or balloon dilation to create the tract. The uncovered intra-hepatic segment of the stent prevents stent migration; to further minimize the risk of migration, two through-the-scope clips (Resolution™, Boston Scientific, Boston, USA) were applied on the duodenal extremity. No adverse events were observed. Jaundice resolved, with no need for further procedures during the follow-up of 5 months.
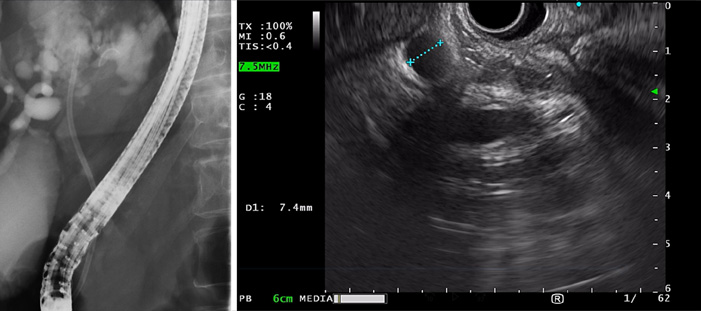
Fig. 2 a Cholangiography after plastic stent replacement in the left hepatic duct. b Dilated right hepatic duct.
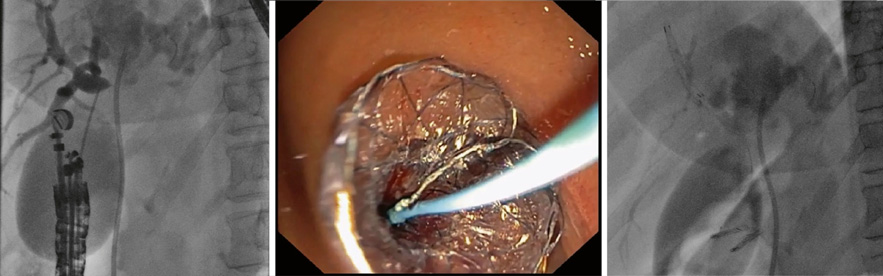
Fig. 3 a Right hepatic duct puncture confirmation by cholangiography. b Hybrid metallic stent placement between the right hepatic duct and the duodenal bulb. c Cholangiography after bilateral biliary drainage with hepaticoduodenostomy in the right hepatic duct and plastic stent on the left hepatic duct.
Percutaneous transhepatic biliary drainage (PTBD) could be an alternative to EUS-HDS in the present case. PTBD requires an external drainage which disrupts the patient’s quality of life, making CERES an internal and elegant solution. Preliminary data of the clinical outcomes of CERES in malignant hilar biliary obstruction have shown significantly lower recurrent biliary obstruction rates compared to PTBD, with a similar complication rate and no significant mortality difference [4, 5].















