A female patient, aged 3 years, was referred to our hospital on account of a persistent history of food impaction dating back to when she was 9 months old. This condition was alleviated through induced emesis, and the patient exhibited limited tolerance for solid foods, exclusively consuming liquids, leading to inadequate weight gain and falling below the third percentile. Notably, there were no reported instances of regurgitation.
A barium swallow test was conducted, revealing a posterior indentation on the upper thoracic esophagus, with a regular progression of the contrast material. This finding suggested the presence of an aberrant right subclavian artery, also known as arteria lusoria. Additionally, stenosis of the distal esophagus was observed, above the phrenic ampulla, characterized by delayed progression of the contrast agent (Fig. 1).
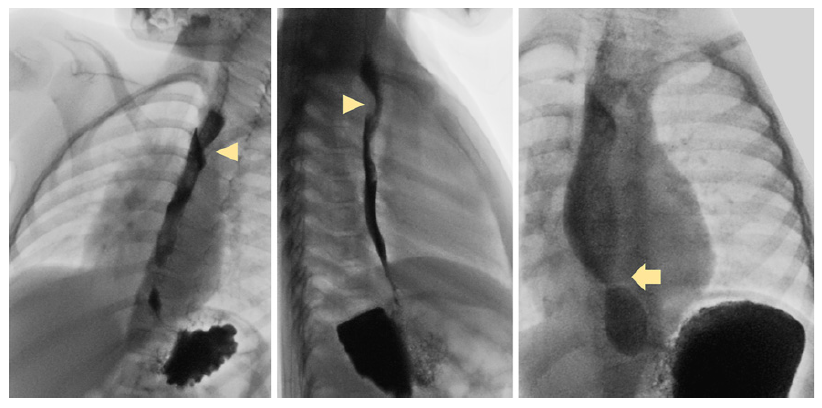
Fig. 1 Barium swallow test with posterior indentation on the upper thoracic esophagus (arrowhead), suggesting the presence of an aberrant right subclavian artery (arteria lusoria) and stenosis of the distal esophagus, above the phrenic ampulla (arrow), with delayed progression of the contrast agent but without complete occlusion.
Esophagogastroduodenoscopy was performed, uncovering, in the upper third of the esophagus, a pulsatile protrusion of the posterior wall. In the distal esophagus, a stenosis was observed, measuring 4 mm in diameter and 2-3 mm in length (Fig. 2). However, passage of an ultra-slim upper endoscope after inflation (5.9 mm) was possible without encountering resistance. The stenosis was found to be untransposable with an 8.8 mm device. Biopsies taken during the procedure did not reveal any pathological findings.
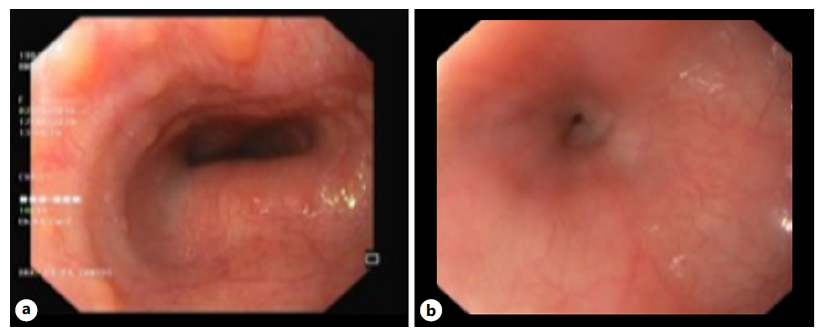
Fig. 2 Esophagoscopy revealing, on the upper third of the esophagus, a protrusion of the posterior wall, pulsatile (a), and, on the distal esophagus, a reduction in esophageal diameter (b).
A CT scan was conducted, confirming the presence of an aberrant right subclavian artery causing esophageal compression (Fig. 3). Two millimetric hyperdense images were observed in the distal esophagus, lacking specific characteristics, without significant stenosis (Fig. 3).
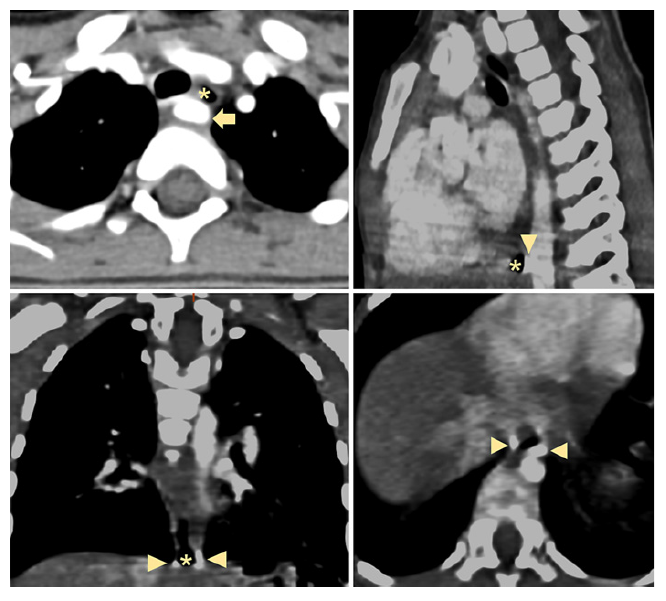
Fig. 3 Chest CT scan shows an aberrant right subclavian artery (arrow), passing around the esophagus (asterisk), with esophageal compression. On the distal esophagus (asterisk), the exam reveals two millimetric hyperdense images (arrowheads), nonspecific, without significant stenosis.
Surgeons performed a distal esophagectomy with anastomosis. Histological examination of the resected esophageal wall revealed nodules of respiratory-type cartilage and seromucous glands, compatible with tracheobronchial remnant (TBR) (Fig. 4). The patient has been asymptomatic for almost 2 years after surgery.
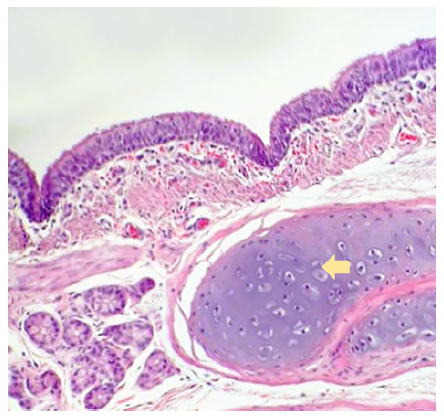
Fig. 4 Histopathology of distal esophagectomy. Ciliated respiratory-type epithelium with a layer of connective tissue, glands, sparse smooth muscle, and a well-defined nodule of cartilage (arrow) (HE, ×200).
Congenital esophageal stenosis (CES) is a constriction of the esophagus present at birth, which may not cause any symptoms in the neonatal period. It is a rare condition. It can be attributed to factors such as TBR, segmental fibromuscular hypertrophy, and membranous diaphragm/stenosis [1]. TBR, also known as choristoma or heterotopy, represents one of the most common causes of lower CES [1].
The etiology is unknown, although an embryologic origin has been suggested. Failure to separate the esophagus from the respiratory tract on day 25 of gestation can halt cartilage growth, typically near the cardia, within 3 cm [2]. CES is frequently associated with esophageal atresia [3].
Symptoms start during the transition from liquid to solid diets and include dysphagia, regurgitation, and vomiting. The severity of these symptoms correlates with the degree of involvement of the esophageal wall [3].
The diagnosis is suspected from clinical, endoscopic, and esophagographic correlation. These exams enable the evaluation of stenosis severity and associated dilation upstream, while ruling out alternative causes of stenosis [1].
Adefinitive diagnosis is only achieved through histopathological examination of the resected esophageal segment, which includes the presence of cartilage, seromucous glands, and pseudostratified ciliated columnar epithelium [4]. Surgical excision, either by resection of the stenotic region or by enucleation of the cartilaginous remnants, is the recommended treatment approach [1, 5]. In cases of CES, diagnostic differentiation is essential, to identify the best treatment.














