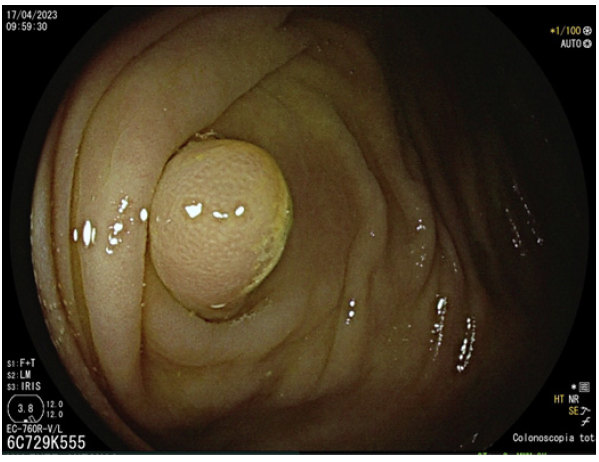
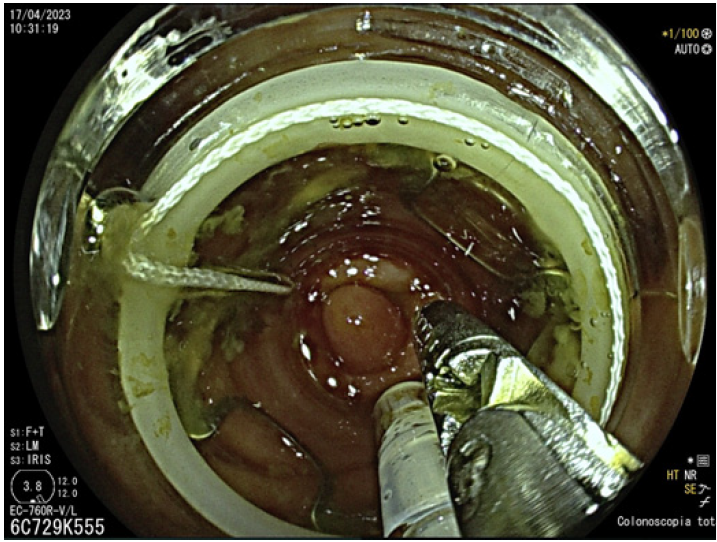
A 71-year-old man with a previous appendicectomy underwent colonoscopy, after a positive fecal occult blood test (by the immunochemical method), that showed a submucosal lesion in the appendiceal stump. He was referred to our department where an abdominal CT scan was requested with no relevant findings identified. A revaluation colonoscopy was scheduled, where a 10-mm polypoid lesion underneath normal-appearing mucosa, consistent with a submucosal lesion, was identified in the center of the appendiceal orifice (shown in Fig. 1). Standard polypectomy or endoscopic mucosal resection was considered not feasible. We proceeded to endoscopic full-thickness re-section (EFTR), using the full-thickness resection device (FTRD, Ovesco®,Germany) (shown in Fig.2, 3).The patient was discharged 1 h after the procedure, with no symptoms. No prophylactic antibiotics were given. Follow-up was uneventful, without complications. Histopathologic analysis of the lesion revealed a sub-mucosal proliferation of smooth-muscle bundles, mature adipose tissue, and thick-walled tortuous vessels, consistent with a diagnosis of a hamartoma with a R0 resection.
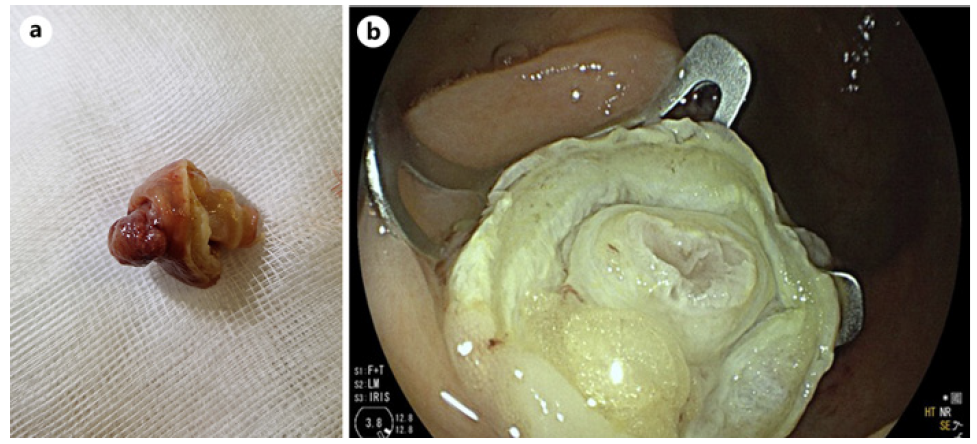
Fig. 3 a Macroscopic image of the resected specimen, with the submucosal lesion on the cecal side, and the appendiceal stump on the opposite side. b Endoscopic aspect of the resection site, with the EFTR over-the-scope clip in situ.
Hamartomatous polyps of the gastrointestinal tract are a rare entity and may be solitary or multiple, the latter often associated with genetic predisposition, such as Peutz-Jeghers syndrome (PJS) and juvenile polyposis. It is vital to distinguish these two identities since the last one involves an increased risk of cancer. Two types of solitary polyps can be identified: Peutz-Jeghers-type solitary polyps that usually appear during the 4th decade of life in patients without family history of PJS and extra-digestive manifestations, such as mucocutaneous hyperpigmentation; and juvenile sporadic polyps, more common in children and mostly located in the rectosigmoid region. Histological diagnosis of hamartomatous polyps is relatively straight forward, but the distinction between particular types may be tricky [1]. In the clinical case here reported, considering the age of the patient, the location of the lesion, and the histology report, a solitary Peutz-Jeghers-type lesion is most likely. There was no familiar history or extra-digestive manifestations that resembled PJS.
Solitary hamartomatous polyps are mostly found in the colon and rarely in the appendix [2], with only a few cases described. They can be asymptomatic and found accidentally or manifest as a complication such as intussusception, which entails a surgical approach [3, 4]. Classically, the primary method of resection of colorectal submucosal lesions was surgery, and an endoscopic approach was not possible for lesions inserted at the inner part of the appendix. Recently, new endoscopic procedures were developed and are gaining more and more acceptance, such as EFTR. This device-assisted technique involves transmural resection of the digestive wall preceded by preemptive clip closure of the future defect. It provides a less invasive approach for management of lesions in the deeper layers of the digestive wall or positioned at complex anatomical sites, such as the appendix, while still achieving clear resection margins [5].
In conclusion, this case highlights a rare identity and the role of EFTR in the management of lesions previously not amenable to endoscopic resection, such as submu-cosal and/or appendicular lesions. Currently, it should already be regarded as an alternative to surgery in selected patients.