Service planning should rely on epidemiological evidence
Dementia is a public health issue worldwide, with a heavy burden of disease and impact on families and informal caregivers [1-3]. In Portugal, official policies have been lacking for decades [4, 5], but efforts were recently made toward a national dementia strategy [6, 7].
Efficient dementia prevention and care delivery call for the implementation of an integrated health and social services framework. A robust evidence base is needed [5], and international reports advise regular updating of epidemiological data [1, 8]. Recently, high-quality research was conducted in low- and middle-income countries [9], whereas in more industrialized regions, where most classic prevalence studies have taken place, we run the risk of becoming outdated. In Europe, epidemiological surveys are nowadays difficult to implement, owing to financial constraints and low participation. This applies not only to costly incidence studies but also to prevalence ones.
Although epidemiological fieldwork studies were inexistent in Portugal until recently, important evidence on the community prevalence of dementia is now available. Regardless, 2 issues remain. First, published Portuguese estimates of numbers of people with dementia have not considered evidence directly stemming from populational fieldwork. Second, should we use findings derived from national samples to estimate those numbers, the results of Portuguese community prevalence studies will differ to a considerable extent. The question remains: why do they differ? In this paper, we aim to address these issues, contributing to the discussion of dementia policies and service planning in Portugal. Mild cognitive disorders are beyond our aim despite their importance as a risk factor for dementia in up to a fifth of older-age people and the need for adequate interventions [8]. Instead, we chose to focus on cognitive decline with consequent social or occupational impairment, i.e., dementia.
Published counts of people with dementia in Portugal
Until recently, Portuguese authors were restricted to indirect methods to estimate the number of people with dementia in the Country. These extrapolations relied on international prevalence rates or expert consensus. A first one [10] was published in 1994, based on EURODEM study results; Garcia et al. estimated 92,470 persons in the general population, 48,706 of them with Alzheimer disease (AD). The EuroCODE consortium provided an updated number of 153,000 in 2008 [11] and Alzheimer Europe reported 182,526 people with dementia aged 60+ years in 2013 [12]. Santana et al. [13] then used the 2005 Delphi consensus rates for the EURO A region [14] to estimate 160,287 people with dementia aged 60 years or older by 2014, as well as 80,144-112,201 people with AD. Others [15] calculated 187,052 in 2020, based again on the Global Prevalence of Dementia consensus [14].
Despite their usefulness, there are obvious caveats with such extrapolations. Paraphrasing Ferri et al. [14]: reliability of international consensus estimates does not ensure validity, particularly regarding regions with fewer populational studies and even if they have originated in countries with sociocultural similarities. None of these calculations built on Portuguese fieldwork, and the inclusion or not of nursing home (NH) residents was not entirely clear. Now that community prevalence studies - their own limitations notwithstanding - are available, an update is needed.
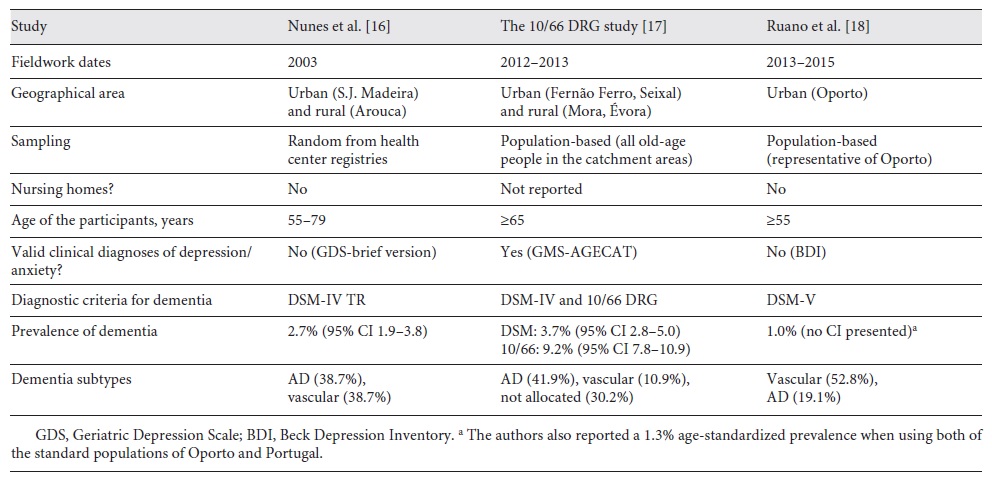
In fact, a 2019 policy report by Alzheimer Europe estimated the total number of people with dementia in Europe and additionally extrapolated per country. Regarding Portugal, this report differed from those mentioned above in that it used raw data combined from studies of national samples [16-18]; 193,516 people living with dementia in the community were estimated [19]. However, the authors did not meta-analyze the national results and it should be highlighted that the 3 studies considered are different in nature (Table 1); pooling their results to produce a single count might oversimplify complex matters. That is why we would now like to discuss the rationale for using our results alone [17] to produce another estimate.
Portuguese population-based studies yield different prevalence estimates
Population-based prevalence direct estimates of dementia are available for selected catchment areas in Portugal (Table 1).
The first study was conducted in the north [16] in 2 samples (urban and rural). The prevalence of dementia was calculated according to the Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV criteria [20] and was 2.7% (95% CI 1.9-3.8). A second field survey was conducted by our group in the south, also in 2 samples (urban and rural) but using the 10/66 Dementia Research Group (DRG) method [17, 21]. The 10/66 DRG is an international consortium, based at King’s College London, whose protocols provide different outputs in terms of dementia case definition not only according to DSM-IV criteria but also according to a regression equation developed in the 10/66 DRG studies [22]. Concerning the prevalence of DSM-IV dementia, the confidence intervals overlapped with the study of Nunes et al. [16], i.e., 3.7% (95% CI 3.0-5.0). However, the prevalence according to the 10/66 algorithm was higher, i.e., 9.2% (95% CI 7.8-10.9) [17]. A third survey was conducted in Oporto and reported a 1.3% estimate for DSM-V dementia prevalence [18].
Besides discrepancies concerning the proportion of dementia subtypes (Table 1), the 3 prevalence estimates are different (especially regarding the results of Ruano et al. [18], even allowing for their use of the most recent DSM version). An obvious question ensues, i.e., what is the explanation for these differences?
Comparing the methods of portuguese prevalence studies
In Table 2, we display additional characteristics (strengths and limitations) of the 3 studies, following the Alzheimer’s Disease International (ADI) quality criteria for prevalence studies [23] frequently adopted in reviews and meta-analyses [1, 24].
Table 2 Three studies on the prevalence of dementia in Portuguese samples: methodological differences according to ADI 2009 criteria
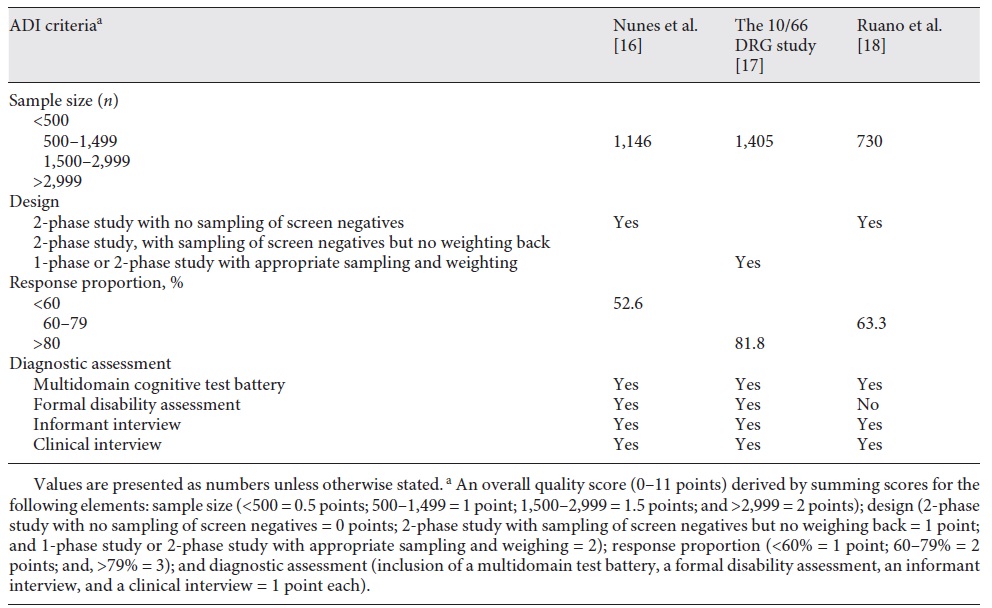
Our study used the 10/66 DRG method. In the last 2 decades, this consortium generated high-quality evidence on the epidemiology not only of dementia but also of mental health, non-communicable diseases, disability, and care dependences [9]. The protocols for prevalence surveys were used in many countries (mainly but not only low- and middle-oncome countries), impacting on research and public health policies worldwide [9].
As detailed elsewhere [17], there were several reasons for implementing the 10/66 DRG method in Portugal. First, following international recommendations [1, 25], we wanted a fixed and fully structured 1-stage, catchment area survey, facilitating international comparisons and reassessments over time. Despite the economic advantages of classical double-phase designs, 1-phase approaches are strongly recommended; there is no attrition bias/informative censoring or need to control for false negatives during screening [1, 26]. Second, we were interested in comprehensive assessments directed not only at cognitive impairment. Psychiatric disorders are crucial for differential diagnosis and their presence may bias estimates of dementia-associated disability and burden of disease. Late-life depression, in particular, has complex relations to dementia; it may be reactive, “homophenotypic”, a prodrome, or a risk factor for dementia, or it may just coincide [27, 28]. In this area, we should not rely on brief rating scales uncritically, especially when cut-off validity cannot be taken for granted [29]. Standardized 10/66 DRG assessments, on the contrary, include, for example, an extensive cognitive module, physical examinations, detailed informant interviews, and the geriatric mental state-automated geriatric examination for computer assisted taxonomy (GMS-AGECAT; a semi-structured interview which is the gold standard in old-age psychiatry epidemiological research) [30]. Altogether, the protocol provides evidence on dementia diagnoses (DSM-IV, ICD-10, and 10/66) and subtypes, mental disorders (“organicity” - including dementia - depression, anxiety, and psychosis), self-reported health conditions and risk factors, disability/functioning (WHODAS 2.0), and service use. Eventually, we were able to assess late-life depression (ICD-10 and subsyndromal depression) [31]. Finally, we wanted to address concerns that DSM criteria may systematically underestimate the true dementia prevalence in low-education, low-awareness settings. The proportion of old-age people in Portugal is now around 20%, and their illiteracy rate is still high [17]. The 10/66 DRG protocol compares DSM-IV caseness against the 10/66 method, which has been proven to be fair in terms of culture and education, in settings not strikingly different from Portuguese rural communities. We acknowledge lacking conclusive evidence of the relative validity of the DSM and 10/66 DRG approaches in Europe, and the current pandemic is delaying our aim of directly establishing the validity of the 10/66 DRG criterion. However, the 10/66 diagnostic algorithm has been extensively validated worldwide [9], and our findings support the concurrent validation of 10/66 and DSM-IV diagnoses [17].
Therefore, we assessed all individuals aged 65 years or older who were residents of mapped catchment areas chosen to reflect nationally typical scenarios [17, 21]. Given the method (design, sampling, and assessment type), the response rate (82%), and the analyzable sample size (n = 1,405), the overall ADI quality score [23] for the study was 10 out of 11 (Table 2). Despite their own limitations [17], these findings provide a better picture of the Portuguese reality than estimates based on studies conducted abroad, seldom on nationally representative samples themselves [32]. Concerning dementia subtypes, 41.9% of the 10/66 DRG cases were diagnosed with AD and 30.2% could not be allocated to pure subtypes [17]. Findings were broadly consistent with pooled estimates of the AD prevalence in Europe (5.05%; 95% CI 4.73-5.39) [33].
The studies of Nunes et al. [16] and Ruano et al. [18] were similar in that they adopted classical 2-phase designs (a screening with cognitive tests followed by detailed clinical assessments of participants screening positive, i.e., probable cases). Both relied on the clinical expertise of clinicians in the second phase; none reassessed a random sample of participants screening negative in the first phase, thereby increasing the probability of “false negatives” and making it impossible to weigh back final results [1, 34]. As ours, their results were not generalizable beyond areas under study and did not target NH, as discussed below. Discrepancies in dementia subtype prevalence estimates are evident, but we would rather focus on dementia syndrome diagnosis, as it is more important for burden of disease evaluation and service planning.
Although the 3 Portuguese studies’ results are not directly comparable, they all contribute to our understanding of dementia epidemiology in Portugal, provided their results are discussed taking methodological options into account. As the 10/66 DRG study reported 2 alternative diagnoses of dementia, and meets most ADI quality criteria, its prevalence estimates may provide an evidence base for estimates of people with dementia living in the community in Portugal.
Updated estimates of people with dementia according to 10/66 DRG results
Overall, the 10/66 DRG study raises important questions regarding policies and services. Which diagnostic criteria are more appropriate to reflect the community burden of dementia: “classical” DSM ones or those of the “epidemiological” and clinically validated 10/66? Moreover, if we were to rely on the latter, how would this shape our estimates of numbers of older people with dementia in Portugal today? Let us start with the second question and take the first one when discussing those numbers.
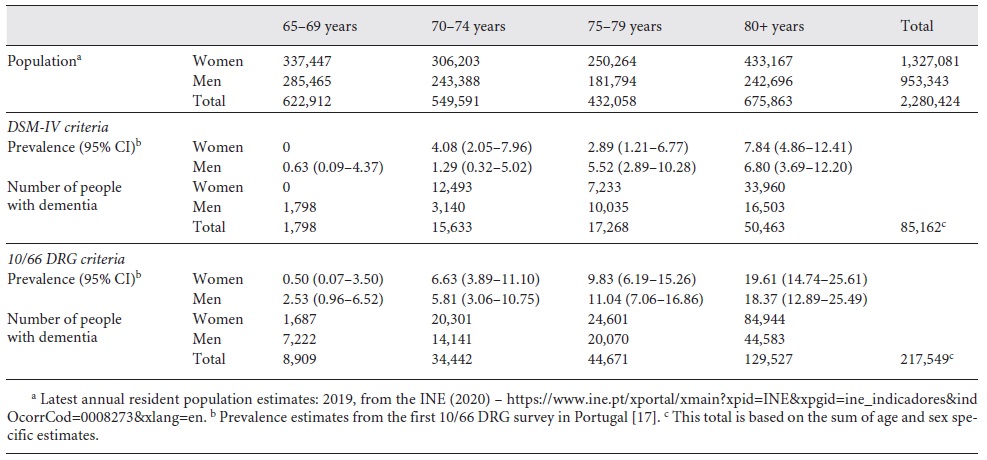
Estimates regarding numbers of community dwellers with dementia in Portugal
We replicated the method of Santana et al. [13] but used age and sex specific prevalence estimates from the 10/66 DRG study [17] to update numbers for the Portuguese older people population in 2019 (2,280,424 residents), as retrieved from official estimates on June 15, 2020 [35, 36]. We did not consider the age interval of 60-64 years, as this category had not been included in our field survey. We considered an aggregate age category of 80 years or older, due to small numbers in our study for those in the separate categories 80-84 and 85 years or older.
Table 3 presents a rough estimation of numbers of noninstitutionalized older-age people with dementia, in Portugal, based on prevalence rates resulting from the 10/66 DRG study (DSM-IV diagnostic criteria vs. the 10/66 DRG algorithm) [17].
Discussion and limitations
When we apply the 10/66 DRG dementia prevalence estimate, previous projections in Portugal (160, 287 [13] to 193,516 [19]) and by the GBD 2016 Dementia Collaborators (166,600; 95% CI 139,562-201,560) [3] are exceeded. Our count (217,549) may even underestimate the total number of people with 10/66 dementia as it refers only to community dwellers, specifically aged 65 years or older. It aligns with the 2015 World Alzheimer Report, with meta-analyzed estimates of dementia prevalence by GBD region, where the age-standardized prevalence for those aged 60 years or older was 6.8% in Western Europe [1]; if people in the age category of 60-64 years had been left out, this would be even closer to our 9.2% prevalence estimate. Our findings are also in line with the 2017 OECD analysis of international data, estimating Portuguese people with dementia in 20 per 1,000 people in 2017 [37]. The same broadly applies to Alzheimer Europe 2019 estimates of 193,516, although their extrapolation of a prevalence of 1.88% regards the general population. Santana et al. [13] used the Global Prevalence of Dementia consensus estimates that included institutions [14] and an official number of 210,581 fewer Portuguese people aged 65 years or older in 2014; this influenced their count in different directions, but discrepancies with our results are most likely due to different prevalence estimates as the basis for calculations.
On the other hand, our lower estimate of 85,162 according to the DSM-IV reopens the debate on which diagnostic framework better conveys the true community burden of dementia, probably undervalued by DSM-IV criteria [9, 38]. Despite their high reliability, numbers generated based on them probably reflect a narrower proportion of more severe cases, failing to consider numerous cognitively impaired and disabled people who would be typically diagnosed with dementia by clinicians but behave as “false negatives” in surveys. This may be especially so in low- and middle-income countries, rural areas, or low-literacy populations due to difficulties in ascertaining cognitive decline and its consequences [39], further supporting the 10/66 DRG approach [17, 21]. Of note, a systematic review and meta-analysis reported an age and sex-standardized community prevalence of DSM-IV dementia of 7.1% in Europe [24]; this is around double of what we found in Portugal [17]. Perhaps the inclusion of our study in the meta-analysis would lower that estimate, probably skewed by some studies restricted to old-old participants [24]. In any case, a single focus on DSM-IV criteria ignores the direction of travel toward current approaches using all available sources of evidence while modeling their potential biasing effects.
We strongly believe that our calculations provide sound evidence-based estimates of considerable numbers of Portuguese community-dwelling people with dementia. The extrapolation builds on fieldwork meeting ADI quality criteria and using structured, transculturally validated methods to foster international comparability. However, this statistical exercise based on a single study is not without limitations. First, the current COVID-19 pandemic is having a direct impact on the mortality of older people, including persons with dementia, which is still evolving. Furthermore, we did not include people younger than 65 years of age and used prevalence estimates not generalizable at a national level. Most importantly, these did not include NH residents. Surprisingly, previous Portuguese estimates do not explicitly address this conundrum.
What about people living in institutions?
Gaps in epidemiological evidence regarding NH hinder dementia policy making. The prevalence of dementia in residential care settings changes from country to country, depending on funding, eligibility, cultural values and norms, the availability of family support, and the propensity of women to work outside the home. It may vary from 13.4% (Hungary) to 70-80% (Sweden) [40]. However, the Alzheimer Europe Yearbook 2017 did not include this estimate for Portugal, where many people with moderate dementia lack appropriate community services and risk precocious institutionalization. In our survey, we did try to evaluate NH residents [21] but realized that the low number of people who could be legitimately accessed with appropriate consent would lead to underestimates of the true prevalence. Hence, we decided not to combine them with estimates of participants living in the community [17]. An overview of our findings is available in the online supplementary material (for all online suppl. material see www.karger.com/doi/10.1159/000516503). Regarding other Portuguese studies, Nunes et al. [16] reported residual cases of institutionalized people with cognitive impairment, and Ruano et al. [18] did not include them.
We use the umbrella term NH as roughly equivalent to the Portuguese ERPI (Estruturas Residenciais para Pessoas Idosas), residential structures for older adults run by nonprofit or for-profit private organizations, sometimes with state funding. They have some nursing staff support and provide higher levels of health and social care than “residential houses”, which are rare in Portugal [5]. Though generally nonspecific to people with dementia, most institutional care for older people is provided by them, and some NGO (e.g., Misericórdias) greatly improved their capacity to support frail residents. Around 3.4% of Portuguese older-age people lived in NH in 2006 [41], but current estimates are 2,526 ERPI and 99,234 residents in Portugal [42]. These figures do not include numerous illegal institutions, probably accounting for around 30.000 residents, or the 4,125 older people supported by the RNCCI (the national integrated continued care network) in long-term and maintenance units in 2019 [43].
Specific estimates of Portuguese NH residents with dementia are very heterogeneous, ranging from 29 to 78% [44-48]. The great variability of these findings derives from differences in aims and methodologies (design, sampling, and assessment tools), but they share their limited scope. In summary, the clinical characterization (including estimation of the dementia prevalence) of Portuguese NH has a long way to go.
What is next?
Debates on trends in the worldwide incidence and prevalence of dementia are ongoing [49]. In high-income countries the incidence may be declining, but evidence is broadly inconsistent regarding changes in prevalence [50, 51]. Regardless, population ageing will probably determine an important increase in numbers of people with dementia [37, 50, 52] and Portugal is expected to have one of the highest percentages of older people in the world by 2030 [53]. We should beware of optimistic projections regarding this public health problem [50] and focus on efficient dementia care policies [5, 54].
Implications for public policies
WHO and ADI advocate global responses to dementia as a public health priority [2, 55]. In Portugal, this requires design and implementation of a true national dementia plan [5, 6]. Given concerns about the limited implementation of guidelines and programs/plans [56, 57], priority choice and feasibility of measures are paramount.
We should avoid multiplying separate programs on different old-age health conditions (e.g., diabetes, cardiovascular problems, and dementia) and instead gain focus by integrating them. Regarding primary prevention, for instance, the potential for dementia incidence reduction was calculated for Brazil, Mozambique, and Portugal by reducing risk factors of dementia over time [58]; these included education, vascular risk, and depression [27, 28]. We could benefit from drawing on recent Integrated Care for Older People (ICOPE) guidelines for the management of decline in intrinsic capacity [59]; these recommendations address decline not only in cognition, but also in mobility, nutrition, vision and hearing, and mood and continence, aiming to prevent or delay the onset of care dependence and promote healthy ageing. Research, including by the 10/66 DRG, supports this framework [60].
Another key issue involves primary care services. This regards early timely diagnosis of dementia and its appropriate disclosure, as well as areas like treatment monitoring, counselling and support, and monitoring of carers’ health [5]. Despite international recommendations on task sharing with neurologists or psychiatrists, coordination and continuity of care in truly collaborative environments is far from being implemented [61].
Implications for research
On the other hand, assessment of the situation involves not only epidemiologic but also service delivery assessments and stakeholder mapping [62]. An exercise to define dementia research priorities clarified that no nation can realistically respond alone to such challenges and advised gaining focus to effectively reduce the burden of dementia [63].
In Portugal, we now have community prevalence data and (despite the scarcity of evidence regarding NH) the societal burden of dementia is uncontentious. Portuguese health services research has highlighted unmet needs in outpatient clinics [64], problems in access and use of community services [65], and the unavailability of information addressing people with young-onset dementia [66]. However, we lack sustainable, feasible methods to monitor trends in prevalence, incidence (including the conversion of minor neurocognitive disorder to dementia) and survival. The same applies to monitoring of diagnosis, treatment, and general management gaps.
So, what should be done now in Portugal? What research needs should be prioritized and how could they be efficiently met? Given all of the evidence now available, and ongoing work from other Portuguese groups [67], timely repetitions of population-based studies using a fixed methodology in defined catchment areas could be more cost-effective than larger-scale projects. For the moment, however, there is a much greater need for evidence regarding dementia prevalence in NH, case finding in health and social services, and the precise care needs of people with dementia and their families, including early-onset dementia.
Specifically regarding institutions, there are barriers to conduction of effective research on the true dementia prevalence. Without adequate design and funding, we cannot generate meaningful estimates from a nationally representative sample of care homes of different types. One additional way to overcome these barriers is to improve the robustness of sampling methods. Low participation due to incapacity to consent when legal representatives are inexistent may be addressed by exceptional ethical and legal approval for epidemiological assessments, on justified grounds.
Characterization of health and social care delivery in dementia is paramount. There is Portuguese research in this area [65, 68-70], but improving information systems, e.g., through access to multisectoral data [62], is still overlooked. Meanwhile, to avoid mismatch of resourcing with true needs, one should keep a critical eye on how widely cited estimations of people with dementia are created [32].
Conclusion
We updated estimates of numbers of community dwellers with dementia in Portugal according to the results of our previous 10/66 DRG survey. These numbers are remarkably higher if we use age and sex specific dementia prevalence estimates according to the 10/66 DRG algorithm. DSM-IV dementia may represent a more specific criterion, restricting the diagnosis to more severe and incontrovertible cases. Both values should be considered cautiously as rough estimates, but they are consistent in that more than half of these people are aged 80 years or older. Notwithstanding the limitations of published community studies in Portugal, including our own, their findings strongly support the urgent need for effective national policies in dementia care. These should include feasible mechanisms to estimate dementia-related needs and responses periodically in health and social systems and at regional and national levels.
Acknowledgement
A. Cardoso, J. Alves da Silva, M. Caldas de Almeida, A. Fernandes, C. Raminhos, C.P. Ferri, and M. Prince were part of the 10/66 Workgroup in Portugal. M. Prince provided helpful comments regarding parts of this paper, and without his support the 10/66 Dementia Research Group Portuguese survey would not have been possible. J. Grave helped editing the tables.
Funding sources
Work leading directly to this paper was not funded. The 10/66 DRG dementia prevalence study in Portugal was supported by FCT (Fundação para a Ciência e a Tecnologia; PTDC/SAU-EPI/113652/2009: “Prevalence of old age neuropsychiatric disorders: contribution to mental health policy in Portugal” - P.I. M. Xavier).