Introduction
Noise pollution has been increasing all over the world, mainly in urban environments [1], due to sources such as road, rail and air traffic [2]. Observational studies in these populations have associated noise exposure with negative effects that go beyond the auditory system [3], and longitudinal cohort studies have shown that noise pollution specifically increases the risk of developing metabolic syndrome [4-6].
Metabolic syndrome is a pathological condition that includes central obesity, insulin resistance (or type 2 diabetes mellitus), hypertension and dyslipidaemia [7], in a complex interaction between individual genetic predisposition and environmental factors [8-10]. Observational studies in cities such as Stockholm and Toronto showed that noise exposure is associated with an increased risk of obesity, hypertension, diabetes and dyslipidaemia [6].
Due to the increased prevalence, morbidity and mortality of metabolic syndrome worldwide [11], particular attention has been paid to environmental determinants, namely noise, to counteract the epidemiological trend [12]. However, observational studies have been carried out in a small number of cities in countries such as Denmark, Sweden, Norway, Canada and the UK, having a limited external validity, as these have specific social, urban and demographic characteristics [6]. Thus, studies are relevant to estimate the association between exposure to urban noise and its cardiometabolic effects in different populations [13, 14].
Lisbon, the capital and largest city (and municipality) in Portugal, has a territory of about 85 km2 and a population of approximately 550,000 individuals, divided into 24 parishes [15]. The population of Lisbon is exposed to high levels of noise throughout the day, originating from road traffic, due to the high volume of daily passengers entering the city [16], as well as rail and air traffic, due to the high number of railway stations and the location of Lisbon airport on the outskirts of the municipality, just 5 km from the centre [16], and with the air corridor cutting the city in half.
This sound environment, characterised by excessive daytime and night-time noise, has changed little since 2008 despite the monitoring and intervention programmes on urban noise in the city of Lisbon, placing Portugal and in particular the city of Lisbon in a very unfavourable situation in terms of noise levels under European air traffic legislation, according to the European Environment Agency [16]. Lisbon is the second-worst rated European capital regarding exposure to air traffic noise, in terms of the Lden indicator (average of 24 h weighted by day, evening and night periods), with 15% of the population in Lisbon municipality exposed to levels above 55 dB, and in terms of the Ln indicator (night noise between 11 p.m. and 7 a.m.), with 10% of the population exposed to levels above 50 dB [16].
To the best of our knowledge, there are no studies that verify the relationship between noise exposure and metabolic syndrome in the city of Lisbon. Therefore, we carried out an exploratory cross-sectional study to evaluate the association between exposure to urban noise and the prevalence of type 2 diabetes mellitus, obesity and hypertension in Lisbon.
Materials and Methods
Study protocol and data provision were approved by the Ethics Committee of the Regional Health Administration of Lisbon and Tagus Valley, IP (ref. 1723/CES/2017). The association between the different variables was verified at the level of each of the 24 parishes (“freguesias”) of the city of Lisbon: Ajuda, Alcântara, Alvalade, Areeiro, Arroios, Avenidas Novas, Beato, Belém, Benfica, Campo de Ourique, Campolide, Carnide, Estrela, Lumiar, Marvila, Misericórdia, Olivais, Parque das Nações, Penha de França, Santa Clara, Santa Maria Maior, Santo António, São Domingos de Benfica and São Vicente.
Urban noise exposure in Lisbon
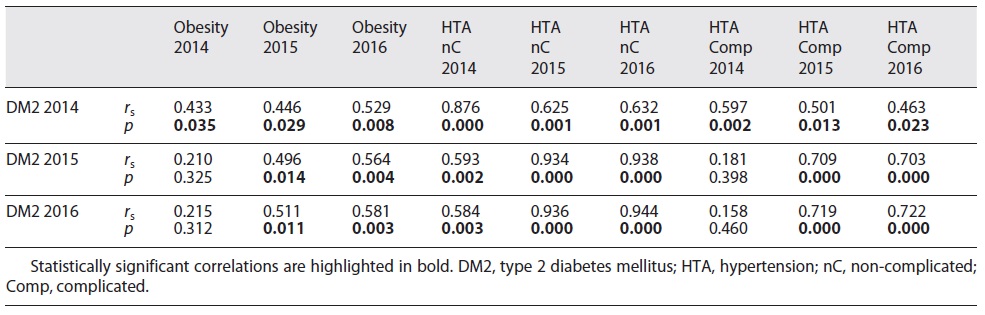
European Directive 2002/49/CE and Portuguese legislation (Decree-Law 146/2006) instructed municipalities to draw up noise maps to assess noise emissions from the road, air and rail traffic in three reference periods - day, evening and night. Since 2008, the municipality of Lisbon has publicly released its noise map, drawn up following legally established criteria (shown in Fig. 1). A detailed description of the development of these noise maps can be found elsewhere [17]. More recent noise maps have shown that noise levels in Lisbon have been similar throughout the years [15].
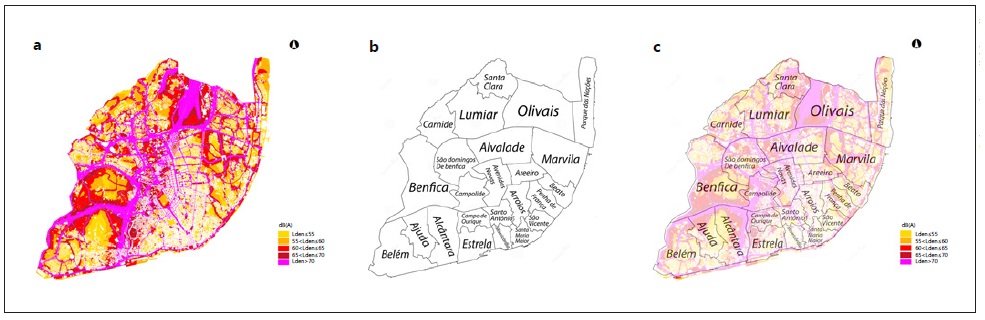
Fig. 1 a Lisbon noise map in 2008 showing the estimated noise exposure for the combined diurnal, evening and nocturnal emissions (adapted from [15]). b Outline of the boundaries of each parish in Lisbon (retrieved from [54]). c Lisbon noise map in 2008 with the outline of the boundaries of each parish in Lisbon (adapted from [15,54]).
For the distribution of noise levels across the 24 parishes of Lisbon, measurements of noise emissions from the 2008 Lisbon noise map were considered for the three reference periods, obtained in the various streets of the city. Each street was assigned to the respective parish, and if a street crossed two adjacent parishes, it was assigned to both. After all streets were allocated, the average noise emissions for each parish were calculated for each reference period. The mean values and standard deviations of noise emission from each parish and reference period are shown in Table 1.
Prevalence of Type 2 Diabetes Mellitus, obesity and hypertension in Lisbon
Data were obtained from the Regional Health Administration of Lisbon and Tagus Valley on the number of adult patients with type 2 diabetes mellitus (identified by the International Classification of Primary Care [ICPC] code T90), obesity (ICPC code T82), uncomplicated hypertension (ICPC code K86) and complicated hypertension (ICPC code K87) in 2014, 2015 and 2016 for each parish in the municipality of Lisbon. To calculate prevalence as a percentage of the population for each parish and each year, the population of each parish of Lisbon in the 2021 census [18] was subtracted from the corresponding data in the 2011 census [18] to obtain the estimated population variation for each parish and each year between 2011 and 2021 (online suppl. material, see https://www.karger.com/doi/10.1159/000520263). As such, the estimated population of each parish in the city of Lisbon in 2014, 2015 and 2016 was obtained (online suppl. material) and prevalence as a percentage of the population was calculated. The prevalence of type 2 diabetes mellitus, obesity, uncomplicated and complicated hypertension in 2014, 2015 and 2016 for each parish is shown in Table 2.
Table 2 Prevalence of type 2 diabetes mellitus, obesity, uncomplicated and complicated hypertension in 2014, 2015 and 2016 for each parish in Lisbon
Statistical Analysis
The non-parametric Spearman’s rank correlation coefficient was used for data analysis using type 2 diabetes mellitus, obesity, uncomplicated and complicated hypertension prevalence in 2014, 2015 and 2016 and diurnal, evening and nocturnal noise emissions for each civil parish as variables. This test was used because deviation from a normal distribution was significant (p = 0.008) for nocturnal noise and strongly suggested (p = 0.059) for evening noise, as shown by the Shapiro-Wilk test of normality. As a surrogate analysis, the parametric Pearson correlation coefficient was also computed for the same associations. The analysis was performed using the IBM SPSS Statistics for Windows software, version 26 (IBM Corp., Armonk, NY, USA), at a significance level of 5% (α = 0.05).
Results
Noise levels in Lisbon decreased throughout the day, with the lowest values observed at night (as shown in Table 1). The noisiest parish in the city of Lisbon for all reference periods was “Santa Clara.”
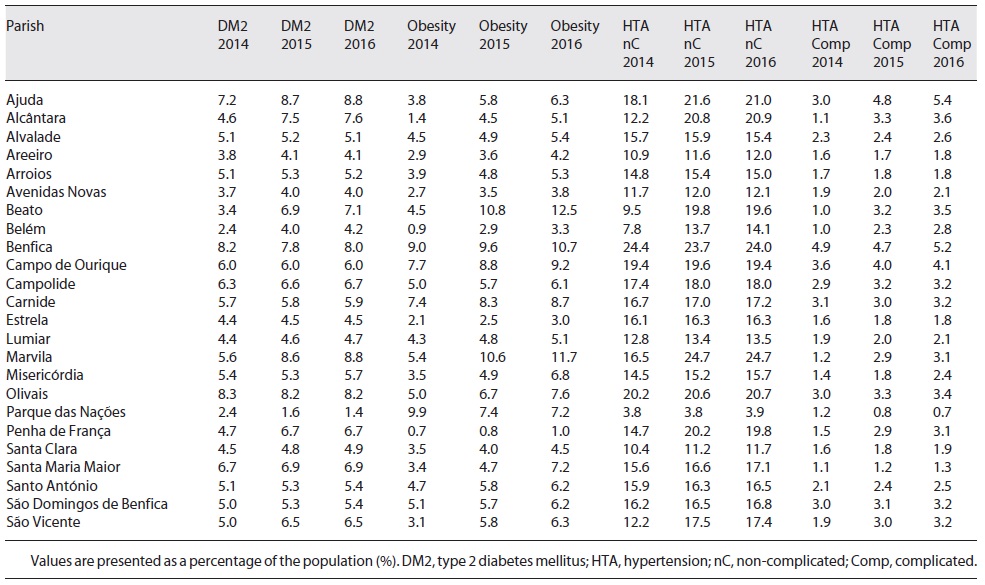
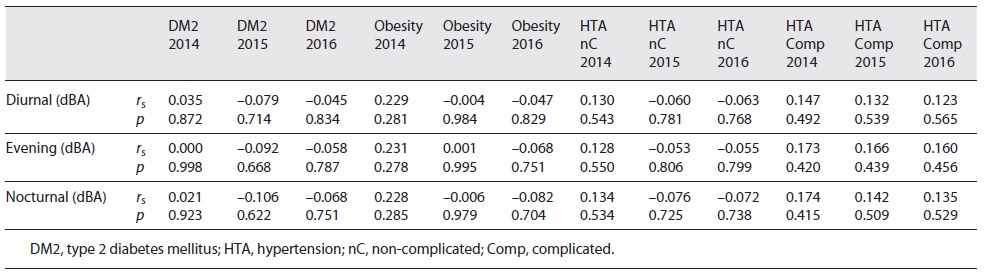
No correlations were found between diurnal, evening or nocturnal noise exposure and the prevalence of type 2 diabetes mellitus, obesity or hypertension in any of the studied years (shown in Table 3). The magnitude and significance of these associations were essentially the same using the Pearson correlation coefficient. Consistent correlations were found between the prevalence of type 2 diabetes mellitus, obesity, uncomplicated and complicated hypertension throughout the studied years, as shown in Table 4.
Table 3 Spearman’s correlation coefficient (rs) and its significance (p) between diurnal, evening and nocturnal noise emissions and prevalence of type 2 diabetes mellitus, obesity, uncomplicated and complicated hypertension in 2014, 2015 and 2016 in the 24 civil parishes of Lisbon
Discussion
Our study aimed to investigate a possible cross-sectional association between exposure to urban noise and the prevalence of type 2 diabetes mellitus, obesity and hypertension in the city of Lisbon. We found no association between the considered factors, unlike other studies where authors found an increased risk of cardiometabolic diseases in populations exposed to noise [19-26].
There is a strong biological plausibility for an association between noise exposure, type 2 diabetes mellitus, obesity and hypertension. Noise exposure acts as a physiological and psychological stressor, activating the neuroendocrine pathways, such as the hypothalamus-pituitary-adrenal axis and the sympathetic nervous system, with subsequent release of cortisol and catecholamines [27]. Long-term noise exposure leads to chronic hypercortisolism and hyperglycaemia and, as such, promotes hyperinsulinism, insulin resistance, dyslipidaemia, central adiposity, endothelial dysfunction, oxidative stress, inflammation and thrombotic predisposition [28-30], which lead to the development of type 2 diabetes mellitus, obesity and hypertension [31, 32]. These effects are particularly pronounced with exposure to nocturnal noise. Nocturnal noise exposure can decrease sleep duration, reduce sleep quality and disrupt circadian rhythm, which is strongly and independently associated with adverse metabolic effects such as obesity and type 2 diabetes mellitus [33-35].
Our study found high levels of diurnal, evening and nocturnal noise in Lisbon. These noise levels were above the legally established limit (Decree-Law 146/2006), which define an exposure limit value of 65 dB for daytime noise and 55 dB for nocturnal noise, and the recent World Health Organization guidelines for environmental noise in the European region [36]. Although we did not find a correlation between the factors, these high noise levels observed throughout the day could lead to an increase in negative cardiovascular and metabolic health outcomes in the future [37].
Analysing our results, it is important to consider that there is a significant number of daily commuters in Lisbon that are exposed to daily noise levels of this city but, if diagnosed with any of the studied diseases, are counted in their respective residential municipality and not in Lisbon. Also, there can be a considerable difference between noise exposure assessments based on the residence and the noise exposure measured by the method we used, allocating streets that cross several parishes and that may have various sound intensities due to their large extension [38, 39].
The cross-sectional design does not allow the establishment of a causal inference between the studied cardiometabolic diseases and noise exposure [40], which may also constitute a limitation. The specific associations between residential transport noise and diabetes arise mainly from longitudinal studies, following up a large population-based cohort of residents in urban regions [41]. Interestingly, this association holds even after adjusting for environmental co-exposures, including traffic-related air pollutants [42-45]. Thus, our study was an exploratory pilot study and aimed to establish preliminary evidence for future studies [40]. This is particularly relevant if we consider that strong earlier evidence exists.
Considering hypertension and obesity, the evidence of a relationship with road traffic noise is quite robust and is dose-dependent [23-25, 46-52]. Although we did not find an association concerning these factors, we should take into account that the prevalence of the studied cardiometabolic diseases in each civil parish of Lisbon was based on electronic health records from primary care. This creates a selection bias, excluding people with difficult access to healthcare and people covered by private insurance [53].
In summary, no association was found between exposure to diurnal, evening and nocturnal noise exposure and the prevalence of type 2 diabetes mellitus, obesity and hypertension in Lisbon. These results highlight the need for further research on the cardiometabolic effects of exposure to urban noise in Lisbon, due to its possible harmful effects on human health.
Conclusion
No correlations were found between exposure to urban noise in Lisbon and the prevalence of cardiometabolic diseases in any of the studied years. Noise levels were above the legally established limit and the recommended environmental noise exposure by the World Health Organization. More studies are needed on the cardiometabolic effects of urban noise exposure in Lisbon, especially longitudinal cohort studies with better cardiometabolic disease data and characterization of noise exposure in each parish of the city of Lisbon.
Acknowledgement
The authors would like to thank Davide Menezes and Eng. Pedro Oliveira for all the help provided with the Lisbon noise map.
Statement of Ethics
This study protocol was reviewed and approved by the Ethics Committee of the Regional Health Administration of Lisbon and Tagus Valley, IP, approval number 1723/CES/2017.
Funding Sources
This research did not receive any funding from agencies in the public, commercial or not-for-profit sectors.
Author Contributions
G.M.P. designed the study, collected and interpreted data and drafted the manuscript. J.B. performed the statistical analysis and revised the manuscript. M.J.O. and P.O. designed the study, interpreted data and substantially revised the manuscript. All authors read and approved the final manuscript.