Introduction
Cancer is one of the main priorities at the European level in health. In this area, the political guidelines of the president of the current European Commission demonstrate and translate into a joint European plan to improve cancer control and optimize care 1.
Head and neck cancer (HNC) has a considerable mortality and morbidity rate, being considered the eighth leading cause of death, and occupying the sixth position among the most common cancers worldwide 2,3. HNC is associated with a heterogeneous group of local malignant neoplasms in the upper respiratory and digestive tract, namely, the oral cavity, hypopharynx, oropharynx, nasopharynx, and larynx 4. There are surgical and nonsurgical treatments, such as radiotherapy and chemotherapy. These treatments can considerably compromise the functional capacity of the person on certain organs intervening in breathing, communication, and feeding, with devastating effects on daily life activities. In this area of the head and neck, the different surgeries performed, such as the larynx (total laryngectomy), the mandible (mandibulectomy), oral cavity (glossectomy), and trachea (tracheotomy), imply physical and psychosocial changes and, commonly, greater dependence on third parties 4.
Rehabilitation as a multidisciplinary practice of oncology care is recent and encompasses a wide range of services, including rehabilitation medical care, in the different physical, psychological, and occupational dimensions 5,6. The Rehabilitation Project of the Portuguese Institute of Oncology Francisco Gentil is coordinated by a specialist in Physical Medicine and Rehabilitation and includes a protocol with many different services. After surgery for HNC, the rehabilitation process is developed by several health professionals. In these two specific services, the multidisciplinary rehabilitation team (physiatrist, rehabilitation specialist nurse, and physiotherapist) holds a weekly meeting to discuss the rehabilitation plans’ implementation and adapt the resources to the patient’s needs. However, for this study, we only considered patients with a rehabilitation nurse (RN) intervention.
An umbrella review demonstrated the effectiveness of a rehabilitation program, improving swallowing function, and mouth opening in HNC patients undergoing multimodal treatment 7. Their swallowing exercises program, which was taught by a multidisciplinary team (speech and language therapists, specialist nurses, and medical professionals), allowed them to address and improve the side effects of multimodal treatment of HNC and led to a better quality of life for patients with HNC 7. Specialist nurses can play an important role in assisting the delivery of oropharyngeal swallowing exercises, including jaw exercises, tongue exercises, and swallowing maneuvers to help improve HNC complications and quality of life for those patients 7. It would also be interesting to know, in addition to rehabilitation in swallowing, what results from intervening in other areas of the rehabilitation process after the surgery of patients with HNC.
In 2010, the Association of Rehabilitation Nurses published a position paper enhancing the importance of RN in the patient’s quality of life and urging for specialized education. RN is an integral part of the multidisciplinary rehabilitation team. They conceive, implement, and monitor differentiated intervention plans, providing care based on scientific evidence 8,9. They bring a unique knowledge base and skill set to the care of cancer patients, founding the intervention in psychosocial support, patient/family education, preventive actions, and plan discharge as early as possible 8
There is already some research on the challenges that patients face after HNC surgery. However, there are no studies demonstrating the RN intervention during the hospitalization of these patients. This is the starting point for this study and the research question: does the intervention of the RN optimize the independence of the patient hospitalized in the head and neck surgery service or in the otorhinolaryngology service? Thus, the main objective was to compare the independence of hospitalized patients who underwent RN intervention versus general health care after HNC surgery.
Methods
An observational and cohort study was designed from July 2018 to October 2020. The data were collected retrospectively, after the intervention of RN in patients between 18 and 100 years hospitalized in the head and neck surgery service or the otorhinolaryngology service (Portuguese Institute of Oncology Francisco Gentil). The identifiable target population were patients hospitalized in the surgery unit with tongue carcinoma, oral pavement, gum, retromolar, larynx, and cervical metastasis, with a non-probabilistic convenience sample of the patients submitted to the different types of surgery under analysis: ganglion cervical emptying (GCE); total laryngectomy + GCE; pelvic gloss mandibulectomy + GCE + tracheotomy; pelvic gloss mandibulectomy + GCE + pectoral muscle flap + tracheotomy. All patients submitted to the surgeries previously referred were considered in our study.
General Health Care Group
The usual care provided to the patients of this group is transversal in these two specific services, in the period after surgery until discharge (online suppl. material; for all online suppl. material, see www.karger.com/doi/10.1159/000527717). The patients selected for this group were all those who underwent the types of surgery already mentioned, and there was the provision of general health care without the intervention of the RN.
RN Intervention Group
The selection of patients for this group was based on the RN availability in this unit throughout the follow of process after surgery until the discharge day. This group includes all patients who, after the surgeries under analysis, obtained evaluation and intervention from the RN, and their eligibility is those whose intervention began in the immediate postoperative period (first 24 h after surgery). In this case, in which the evaluation (first 24 h) and the first intervention are made, the initial Barthel Index, which translates the independence soon after surgery was considered. The RN interventions in these two surgical specialties are described in online supplementary material I.
Data Collection
The data were collected from the national database Homogenous Diagnosis Group (GDH, Grupo de Diagnóstico Homogéneo) ICD-10® and ICD-11® and from the rehabilitation nursing database of both services. In this database, each episode of patient hospitalization is associated with a diagnosis and surgery performed on a given patient, demographic data, time of hospitalization, primary and secondary diagnosis, the occurrence of death during hospitalization, and referral to hospital discharge.
The information on the Barthel Index (initial, discharge), was collected retrospectively by consulting the Excel® database of the RN. The assessment of the initial Barthel Index (first 24 h after surgery) was performed by the RN in observation room. However, when they were not present, the scale was applied by the general care nurse who was in the direct health care of that patient and was experienced in the application of this scale. The assessment of the independence was performed by RN, applying the scale on the day of clinical discharge. In this second database under the responsibility of the RN of this unit, each patient has associated with their hospitalization episodes, so the information of the GDH database, mentioned above, was easily crossed.
Analysis
The variables were organized: demographic characteristics (sex and age); immediate postoperative status in the first 24 h (type of surgery, initial Barthel Index); mediate/late postoperative status after 24 h until discharge (infection, number of days of hospitalization, independence). The Barthel Index is a scale that translates the result of the evaluation performed by the health professional on the patient’s capacity for self-care and has already been validated in the country in which this study was conducted 10. The Barthel scale translates the independence with a continuous value; however, the variable was used as a binary at the time of the discharge showing a difference in dependence/independence of the patient 11. The numerical dependent variable was categorized into dependent or independent. A value greater than 91 points in the Barthel Index at the discharge time translates into independence to carry out daily activities. In contrast, a value below corresponds to moderate and/or high dependence of the patient 11.
For numeric variables, measures of central tendency, mean and median, and of dispersion, minimum, maximum, and standard deviation were determined for the group with intervention and the group of geriatric health care. Frequency distribution tables with the counts and their percentages for both groups were also presented.
The χ2 test was used for categorical variables in the comparison of groups. In the case of numerical variables, the assumptions for performing the Student’s t Test for independent samples were evaluated, and when the criteria of homogeneity of variances and normality were not met, the Mann-Whitney U nonparametric test was chosen to compare the two groups. The level of significance considered for the test result was 5%.
To measure the effectiveness of the intervention on independence, we adjusted the model for initial Barthel Index and age according to the causal model assumed (online suppl. material II). To analyze the effect of the RN intervention on independence a generalized linear model, with a Poisson distribution, and robust standard errors were used. The Poisson model was used because it was an observational study with a prospectively evaluated intervention, with data being collected retrospectively after this intervention. The advantage of this approach is that it readily provides covariate-adjusted risk ratios and associated standard errors 12. Relative risks (RR) and the corresponding 95% confidence intervals (CI) were estimated for RN intervention. The relative risks were adjusted for the variables, initial Barthel Index and age (confounding factors), after analyzing the relationship of all variables on the DAGitty platform 13. DAGitty is a browser-based environment for creating, editing, and analyzing causal diagrams for minimizing bias in epidemiology and other disciplines. The SPSS Statistics software was used for data analysis. The reporting guideline that has been followed in this study is the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE).
Ethics
The study protocol was approved by the Research Unit and the Health Ethics Committee of the institution with the number UIC/1427. The information was collected retrospectively, not being possible to obtain any contacting or locating element of the participants in the aforementioned databases, all the information used and collected in the context of this study was analyzed in a coded and confidential manner, being each episode of hospitalization transcribed to a corresponding code (1, 2, 3, …) in order to maintain the confidentiality and anonymization of the collected data. Only the investigator of this study will have access to their identification by the code that has been assigned. Registration was performed on the clinical trial platform, ClinicalTrials.gov.
Results
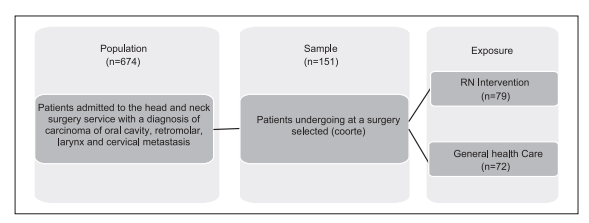
The identifiable target population has 674 patients hospitalized in the head and neck surgery service or the otorhinolaryngology service submitted to the surgeries mentioned above (Fig. 1). There were 85 patients who died until the date of data extraction, 368 who had other surgeries than those mentioned, and 70 whose results were impossible to obtain, which were not included in the study. The sample studied has 151 patients, 79 who underwent RN intervention and 72 who were in general health care after surgery. It consists mainly of men (n = 129, 85.4%), tending to be older with a mean age of 66.5 years, with half of the sample being at least 67 years old.
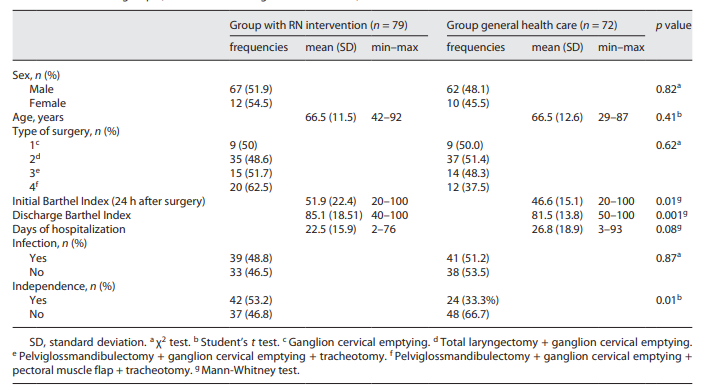
Comparing the two groups (RN intervention vs. general health care), there were no statistically significant differences concerning demographic characteristics (age, gender, and age group), type of surgery, and infection (Table 1). More than half of the patients (66,7%) who received general health care were not independent at the time of clinical discharge (p = 0.01). 53.2% of the patients who underwent intervention by the RN were discharged as independent in the activities of daily living, according to the variable independence (p = 0.01).
To evaluate the effect of RN intervention on independence, a Poisson regression model was used, adjusting for initial Barthel Index and age (Table 2). After the regression model, it should be noted that the effect of the independence according to the intervention of the RN is estimated at 1.59 (95% CI: [1.08; 2.34]; p = 0.01). However, when adjusting for the initial Barthel Index (MOD1), the effect is no longer statistically significant (RR: 1.32; 95% CI: 0.92; 1.89]; p = 0.13). When adjusting for the initial Barthel Index and age (MOD 2), the intervention of the RN becomes effective for the independence (1.47; 95% CI: [1.02; 2.12]; p = 0.03) of the patient undergoing head and neck surgery.
Table 2 Relative risk of the independence after discharge between patients submitted to RN intervention versus general health care

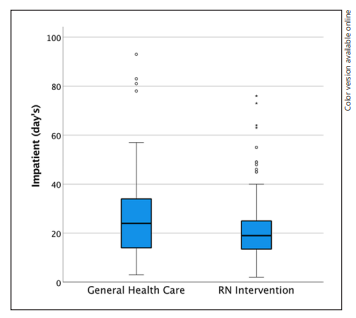
Regarding the days of hospitalization, the mean length in the RN intervention group (22.5 days) was lower than the mean of the general health care group (26.8 days) (Fig. 2). There was an average reduction of 4.3 days (26.8 days - 22.5 days = 4.3 days) in the group in which the RN intervened, although statistical tests did not reveal significance (p = 0.08).
Discussion
The main consequences triggered by elective surgical treatment of HNC patients include dependence and impairment of their functional capacity. Our study found that patients who received only general health care were discharged with a moderate/high degree of dependence. However, patients who underwent RN intervention were discharged independent or with mild dependence. The RN intervention allows an effective recovery of HNC patients submitted to surgery, showing that the intervention of RN through rehabilitation programs promotes independence after his surgery.
The treatment of patients with HNC can compromise their functional and self-care capacity 14-18. Both stiffness and neck pain is associated with the period after surgical treatment, even when cervical ganglion emptying with preservation of the accessory spinal nerve, and early start rehabilitation is absolutely necessary for preventing functional capacity limitations 14. The American Cancer Society recognizes changes in shoulder functionality as a recurrent consequence of this surgery and recommends that patients be referred to a professional specialist in rehabilitation in order to minimize pain, improve shoulder functionality and range of motion, as well as the ability to perform daily life activities 19. In our RN program, the specialist nurse intervened in the specific case of patients undergoing cervical ganglion emptying, to reduce the scapulohumeral pain, improve the shoulder range, and strengthen local muscles.
Rehabilitation should be offered to all patients with HNC, focusing on education after surgery on how to care for themselves in this postoperative period in need of adaptation strategies, including subjects as diverse as advice on maintaining appearance and self-care safely 6. Strategies that include early mobilization and specific rehabilitation programs in HNC surgery allow effective functional recovery and a high degree of independence after surgery 20. Early postoperative mobilization in patients with HNC undergoing flap reconstruction favors better surgical results, contributes to the prevention of cardiorespiratory and muscle complications, promotes gait and independence readaptation, and facilitates the transition process and their recovery at home 21. A study evaluated the effects of a specialized nursing program on patients with HNC on an outpatient basis, which aimed to deal with physical and psychological problems and social consequences of the disease and treatment. After 1 year of intervention (6 counseling consultations every 2 months), patients had a significant improvement in physical terms, pain control, swallowing, social contact, and depressive symptoms 7,15-18,20-22. Although this program was applied to patients followed on an outpatient, the authors refer to the importance of health education sessions after clinical discharge. Our RN program considers this aspect, such as health education sessions on topics such as inhalation therapy management, effective management of respiratory symptoms, and promotion of empowerment, facilitating adaptation after clinical discharge.
Important characteristics as associated with postoperative complications and functional decline in patients undergoing major head and neck surgery. Elderly patients with HNC are often considered poor candidates for surgical treatment owing to impaired functional status and preexisting comorbidities 23. In a retrospective cohort study of patients undergoing major head and neck surgery who received free tissue transfer or pedicle flap reconstruction, we describe rates of 30-day complications, mortality, and functional decline 23. These patients experienced a decline to dependent status, and a multivariable analysis showed a higher risk for 90-day functional decline after additional surgical procedures over hospitalization 23. In our RN program, elderly patients were also considered (Table 1), in which the range in the age was 42-92 years and a mean age of 66.5 years. Early self-care rehabilitation plays a key role in the physical and psychosocial recovery of HNC patients surgically treated. It is important to consider an early physical rehabilitation program in patients surgically treated because it improves mobility, prevents complications, reduces pain, and widely improves the quality of life.
Our study showed a reduction in the days of hospitalization with the intervention of the RN after surgery, however, this difference was not statistically significant. Rehabilitation programs in patients undergoing HNC surgery optimize functional capacity, reduce complications, and enable earlier hospital discharge 20. Scientific evidence shows that implementing physical exercise programs in patients with HNC, submitted to surgery, enhances recovery in terms of functionality and improvement of quality of life 18. In addition to the benefits resulting from the implementation of postoperative exercise programs, a significant reduction in hospitalization time in patients who additionally performed an individualized exercise program was found to be independently performed 17. Like our RN program, this program enables earlier hospital discharge with the application of active mobilizations after surgery in a patient with HNC.
The intervention of the RN has an effect of improvement in the patient’s independence after surgery, remaining when it adjusts to the Barthel Index and age in the immediate postoperative period. There is no evidence from other studies on the intervention of RN after HNC surgery; however, it is known that age and comorbidities associated with each patient trigger higher dependency with a decreased functional capacity 16.
Health providers, like nurses, empower patients and their caregivers, as well as encourage them to obtain health behaviors based on therapeutic protocols 24. Nurses of general care and specialist nurses have a strategic position due to their proximity to the patient, regularly checking the motivation, and operationalization the plans make for each situation 24. The initial assessment performed by the RN after HNC surgery, based on the implementation of individualized plans, allows for monitoring the evolution of the patient throughout his hospitalization and respective preparation for discharge. The care provided by RN, due to its differentiated and differentiating characteristics, aims to improve and maximize the patient’s function and independence, taking care of themselves according to their activities of daily living.
One of the limitations of the study is related to the evaluation of the initial Barthel Index since when the RN does not perform the intervention, the assessment of the independence was made by the nurse (general health care) who was in the direct provision of care to that patient. The assessment conducted by the RN might lead to the early diagnosis of potential problems associated with HNC surgery, thus intervening early on with preventive rehabilitation nursing actions and promoting independence. Another limitation is related to the non-probabilistic convenience sample and the data collected retrospectively. In future studies, a larger sample will be important.
Conclusion
This study shows the importance of RN in this type of care, promoting an effective recovery of HNC patients submitted to surgery. It is an innovative study on patients after diagnosis of HNC, showing that the intervention of RN through rehabilitation programs allows independence after his surgery. Early self-care rehabilitation for patients undergoing surgery with HNC is essential, considering the role of the RN in the multidisciplinary team, improving health quality indicators for the care provided.
Statement of Ethics
This study protocol was reviewed and approved by the Ethic Committee. Written informed consent does not apply in this study, an aspect validated by the Ethics Committee.
The information was collected retrospectively, not being possible to obtain any contacting or locating element of the participants in the aforementioned databases, all the information used and collected in the context of this study was analyzed in a coded and confidential manner, in order to maintain the confidentiality and anonymization of the collected data. This study protocol was reviewed and approved by the Ethic Committee of the Portuguese Institute of Oncology of Lisbon, approval number [UIC/1427].
Author Contributions
Conceptualization, methodology, and writing - original draft preparation: J.M.; validation and supervision: P.S. and B.N.; formal analysis and visualization: J.M. and P.S.; investigation: J.M. and S.G.; resources: S.G.; writing - review and editing: P.S.; all authors have read and agreed to the published version of the manuscript.
Data Availability Statement
The data that support the findings of this study are available from the Portuguese Institute of Oncology of Lisbon. Restrictions apply to the availability of these data, which were used under license for this study. Data are available from the authors José Moreira and Sandra Gomes with the permission of the Portuguese Institute of Oncology of Lisbon.