Introduction
Cutaneous squamous cell carcinoma (cSCC) represents the second most common nonmelanoma skin cancer (NMSC), the first being basal cell carcinoma. According to the Global Cancer Observatory, the incidence of NMSC in Europe has been reported to be 16.0/100,0001. However, in Portugal, there is a study reporting an average yearly incidence estimation of 91.6/100,0002. The incidence of the cSCC has been increasing over the past decades3 and it's thought to be related to higher levels of sun exposure, an increase in the ageing population, increased sunbed use, and improved skin cancer detection4,5. Although the first treatment approach of these patients is usually surgery, radiation therapy has also an important role in their management either in a curative, adjuvant or palliative setting. We present the case of a woman with an extensive periorbital cSCC with no physical conditions to make an appropriate radiation therapy with adequate positioning in the treatment table. The treatment was considered of great importance to improve patient's quality of life and therefore an unusual approach was taken, treating the patient directly in the hospital stretcher with a direct electron beam of 6 MeV and dose distribution calculated in water.
Case report
An 88-year-old woman presented with a progressively growing skin lesion on the left periorbital area for around 1–2 years with approximately 1 × 1 cm. In May 2018 a biopsy revealed a well differentiated cSCC.
She had a low performance status with a previous medical history of high blood pressure, hyperuricemia, dyslipidemia, ischemic stroke in 2017, and surgical history of osteosynthesis due to left trochanteric fracture. The patient was bedridden with reduced social contacts.
Due to the low performance status, treatment with topical Imiquimod was initiated in June 2018 but stopped just one week later on the recommendation of the nursing home doctor. The patient was next submitted to 2 cycles of 20 seconds each of cryosurgery in July 2018 but one month later she presented to the dermatology appointment with an increase in size and ulceration of the lesion. Mostly by pressure from family members the patient was proposed to another 7 cycles of cryosurgery which overall resulted in a reduction of the size of the lesion.
In December 2018 the lesion progressively increased in size and in a multidisciplinary tumor board discussion, the radiation oncology department was called to assess the possibility of palliative external radiation therapy.
The patient presented at the radiation therapy department with a very low performance status, with low social contacts and in a wheelchair. There was an ulcerated mass in the left periorbital area with about 4 × 4 cm and by that time it was impossible to visualize the eye or open the eyelid (Fig. 1). The patient was submitted daily to disinfection and dressing of the lesion with considerable pain.
Planning computed tomography was performed in our department in a right lateral decubitus position with adequate immobilization of the head using a thermoplastic mask connected to a base plate. External marks were placed on the mask for laser alignment. Computed tomography images showed no evident invasion of the left eye.
First, we performed a three-dimensional conformal radiation therapy plan with 6-Mv photons and a 5-mm bolus covering the lesion with a gross tumor volume (GTV) planning to target volume (PTV) margin of 3 mm due to the location and size of the lesion. A total dose of 30 Gy in 5 fractions was prescribed.
On the first treatment fraction, as the patient was not able to tolerate the position needed for the treatment table due to continuous agitation, treatment was stopped.
Because of the progressive lesion growth despite previous treatment attempts, it was assumed that the treatment was mandatory to improve patient's quality of life. Therefore, it was decided to make a two-dimensional treatment with direct electron beam and a 5-mm bolus over the lesion, on the hospital stretcher (Fig. 2) with a fractionation scheme of 30 Gy in 5 fractions (6-Mev electrons) given with at least 2 days of interval and dose distribution calculated in water.
The patient was able to complete the second proposed treatment with no interruption or delay and without relevant side effects.
On the first follow-up appointment in February 2019, two weeks after finishing the radiation therapy treatment, the patient presented with a partial response, with clinically visible mass reduction and a decrease in pain (Fig. 3).
On the second appointment, six weeks after the radiation therapy, the lesion was progressively reduced in size, the eye was now visible and there was great pain reduction.
In April 2019, eight weeks after the radiation therapy, clinical response was almost complete (Fig. 4A).
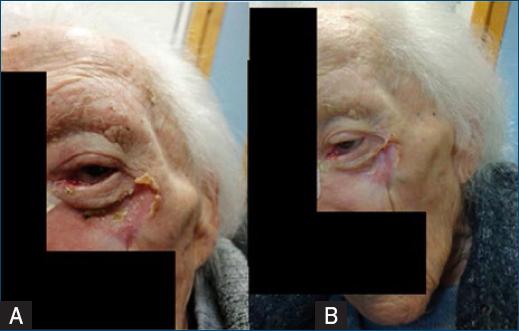
Figure 4 A: lesion 8 weeks after radiation therapy, with complete remission. B: lesion after 4 months after radiation therapy, with complete remission.
In June 2019 there was a complete remission (Fig. 4B). The patient remained in follow-up with appointments in the dermatology department and the radiation therapy department without a recurrence of the lesion until May 2020 when she died from community-acquired pneumonia and cardiac insufficiency.
Discussion
Cutaneous squamous cell carcinoma (cSCC) is the second most common NMSC accounting for 20% of skin cancer12. Incidence trends since the 1940s show a stronger increase in NMSC than in melanoma13, but a large worldwide variation exists on the incidence of cSCC with the highest rates seen in Australia and the lowest reported in Europe14.
The most significant risk factors resulting in cSCC include ultraviolet (UV) exposure, older age, fair skin, and immunosuppression. UV from the sun or tanning beds induces skin cancer by causing DNA damage12, eventhough a european study suggested an association of sunbed use with nevus count, atypical nevi, lentigines, and suspicion of melanoma but no correlation was found with the suspicion of NMSC15. About 65% of cSCC arise from preexisting actinic keratosis6.
In Portugal, the median age for patients with cSCC is 80 years and the face is the most common location accounting for 61.3% of the cases2. cSCC presents as a non-healing, usually progressively enlarging erythematous papule, plaque, or ulcer. Lesions that are painful, grow rapidly and bleed on contact are usually rapidly invasive and carry a higher risk of metastasis7.
High risk factors associated with poor prognosis, recurrence, and metastasis, include tumor size ≥2 cm, tumor depth >6 mm, invasion beyond the subcutaneous fat, poorly defined borders, rapidly growing tumor, location on the “mask areas” of the face, poor histological differentiation, perineural and lymphovascular invasion, and immunosuppression8-10.
The primary treatment objective is to remove the tumor completely with minimal functional and cosmetic impairment, but treatment options differ according to the tumor risk factors. A multidisciplinary consultation should be done in all patients with high risk features8.
For low risk lesions standard excision, Mohs micrographic surgery, curettage and electrodesiccation, cryotherapy or radiation therapy can be chosen8. For high risk lesions Mohs micrographic surgery, standard excision with wider margins and, for non-surgical candidates, radiation therapy with or without systemic therapy or systemic therapy if curative RT is not feasible8. Alternative treatments like topical 5-FU, topical imiquimod, photodynamic therapy or vigorous cryotherapy are used in in situ cSCC or in pre-tumoral lesions.
Radiation therapy can also be used in an adjuvant setting particularly if cSCC shows extensive perineural, large nerve involvement or if excision margins are not tumor free8. Radiation therapy is an effective curative treatment for cSCC, mostly preferred in the head and neck region especially for the nose, eyelids, and ears with 5-year local control of 92% and 10-year local control of 87% with a superior cosmetic outcome when compared to surgery9. Radiation therapy has also an important role in the palliative treatment of neglected lesions in reducing the size of the lesion, the depth of invasion, the hemorrhage, reducing the pain, and overall improving patient quality of life.
The mortality rate associated with cSCC is around 1.5% and the metastization rate is 4%11. Most deaths result from uncontrolled loco-regional recurrence and not from distant organ metastasis9. When deep invasion and eventual metastasis occur, local and regional lymph nodes are the most common sites of metastasis.
In this article, we report the case of an elderly woman with a large cutaneous periorbital SCC who, after no response to cryosurgery was proposed to palliative radiation therapy. Due to the patient's bad performance status and inability to be steady with an immobilization mask in the treatment table, the patient was treated in the hospital stretcher with 2D technique and dose distribution calculated in water.
Conclusion
The first treatment approach of cSCC is usually surgery, but radiation therapy has also an important role either in a curative, adjuvant or palliative setting presenting as a safe, well-tolerated, and effective treatment.
We report this case to contribute to enrich the discussion about the need to understand and keep in mind older radiation techniques that might still play an important role in the treatment of specific patients, due to a greater freedom of treatment positions. Often it is the only possible treatment option with good results and low acute effects. In this case, using older radiation therapy techniques, a complete clinical response was achieved in a patient who would otherwise be considered untreatable, and, more importantly, with an improved quality of life, with no pain or need for daily dressings. Also, in these settings, it is useful to use more hypofractionated regimens for greater patient adherence.
Although we are facing a continuous evolution of linear accelerators, special radiotherapy techniques and increasingly effective immobilization systems enabling us to decrease very significantly the dose in organs at risk, we need to rethink our strategy and use older techniques to be able to treat some patients, like the present one.

















