Introduction
In March 2020, the World Health Organization classified the SARS-COV2 virus outbreak as a pandemic event. During the following weeks and months, hospitals and health services were overwhelmed with COVID-19 patients, and society itself went through major changes in order to (try to) contain the virus.
Months before the arrival of the first vaccines, personal protective equipment, frequent hand disinfection, social distancing, and mobility restrictions were the only available means to limit viral spreading. The Dermatovenereology Department of Hospital de Santo António dos Capuchos (HSAC) in Lisbon is in a unique situation in Portugal as it is responsible for all inpatient consultations and urgent outpatient evaluations in Centro Hospitalar Universitário de Lisboa Central (CHULC). Besides HSAC, the Center also encompasses Hospital de São José (HSJ), Hospital Curry Cabral, Hospital Santa Marta, Hospital Dona Estefânia, and Maternidade Alfredo da Costa.
In order to maintain assistential activity while ensuring social distancing and mobility restrictions imposed between hospitals, teledermatology platforms were employed. These can be defined as the use of electronic communications applied to dermatology to exchange medical information between remotely located health care professionals1.
In order to accomplish this, an e-mail address hosted by CHULC’s private network was created and a smartphone was made available to all department physicians. The latter was used both for accessing the previously mentioned e-mail account and also to receive short message services (SMS) and messages through encrypted communication services (such as Whatsapp®). Communication through both of these methods was made available to all physicians in CHULC.
The General Data Protection Regulation was followed in all processes, as patients gave consent to clinical image taking and sharing between medical professionals and patient’s identification relied only on the hospital’s patient ID number (which can only be accessed by medical professionals). Regarding the use of third-party software, consent from patients was also obtained previously; the use of encrypted end-to-end solutions meant that internet service providers, application service providers or any other entity were unable to access information that was only available to the sender and receiver (both medical professionals).
This study aims to evaluate the use of teledermatology methods in CHULC during the COVID-19 pandemic, with emphasis on type and quality of received information, response timing by physicians, and conversion to in-person evaluation.
Methods
A retrospective study of all inpatient and urgent outpatient consultations using teledermatology platforms during a 13-month period was conducted.
All written communications received via e-mail or smartphone between April 1, 2020 and April 31, 2021 were reviewed. Those containing inpatient and urgent outpatient consultations were included. Exclusion criteria were lack of patient identification and the inability to access sent clinical images.
Clinical information was evaluated regarding essential anamnesis and other relevant data. Clinical images were analyzed based on framing, contrast, lighting, color, and sharpness. Data that enabled medical interpretation and decision-making (as defined by a panel of four physicians) was classified as “adequat”. and the remaining as “inadequat”.
Results were analyzed by SPSS Statistics 25®software.
Results
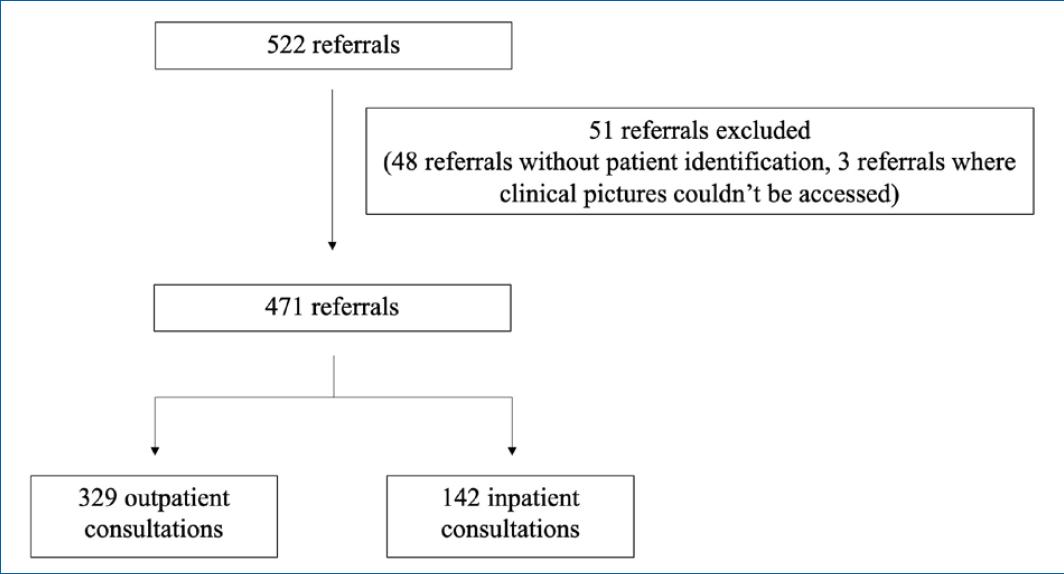
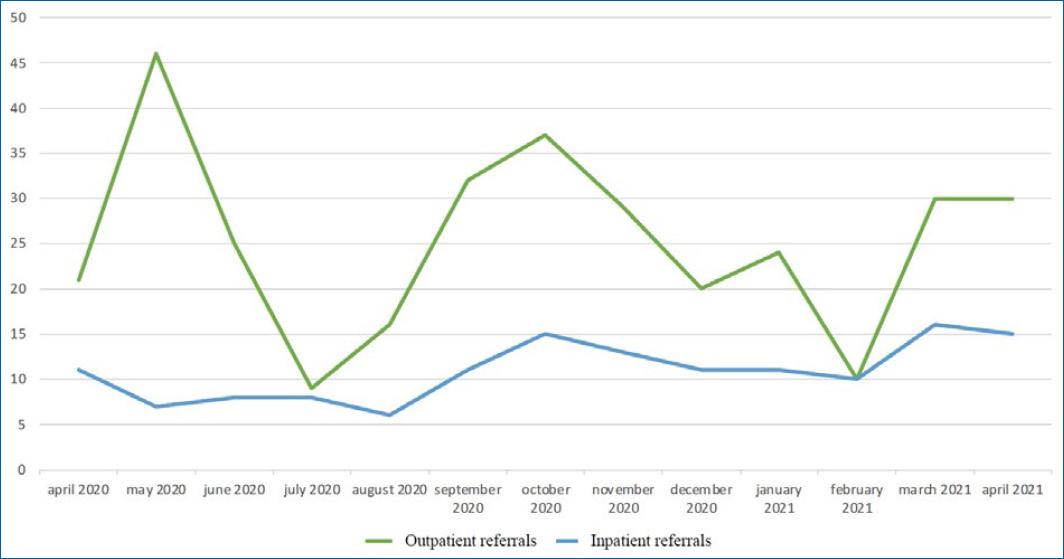
The inclusion criteria were met in 522 referrals and 51 cases were then excluded. Of the remaining 471 referrals, 329 (69.9%) were urgent outpatient consultations and the remaining 142 (30.1%) urgent inpatient consultations (Fig. 1). The distribution of referrals during the 13-month period is shown in Figure 2.
Referred patients had an average age of 53.7 years (1 month–96 years) and 237 (50.3%) were male. Subgroup analysis revealed an average age of 48 years (2 months–96 years) and of 67 years (1 month–94 years) for outpatients and inpatients, respectively.
Most referrals were received through e-mail (324 [68.8%]) and the remaining through encrypted smartphone apps (147 [31.2%]).
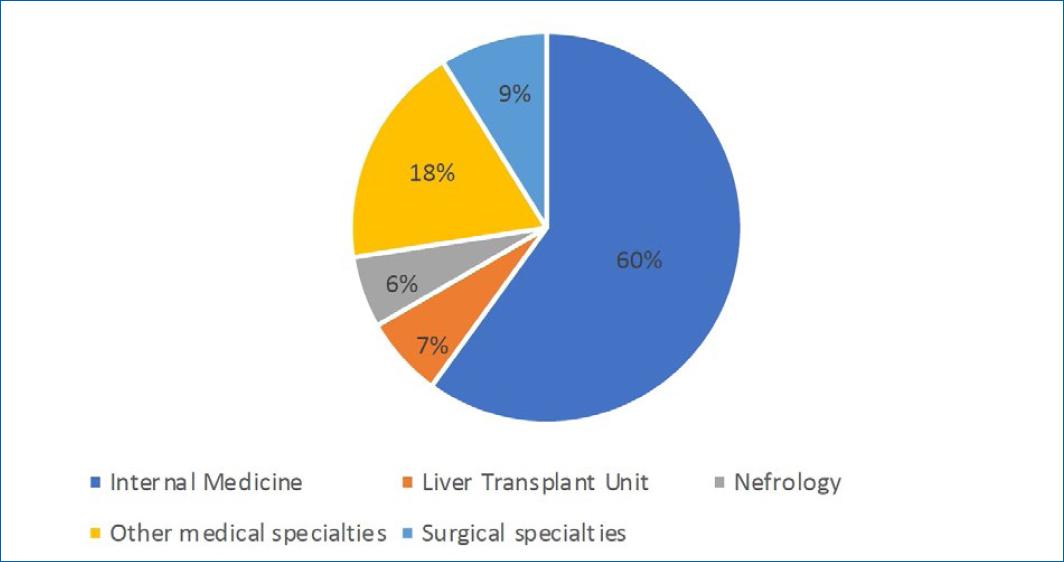
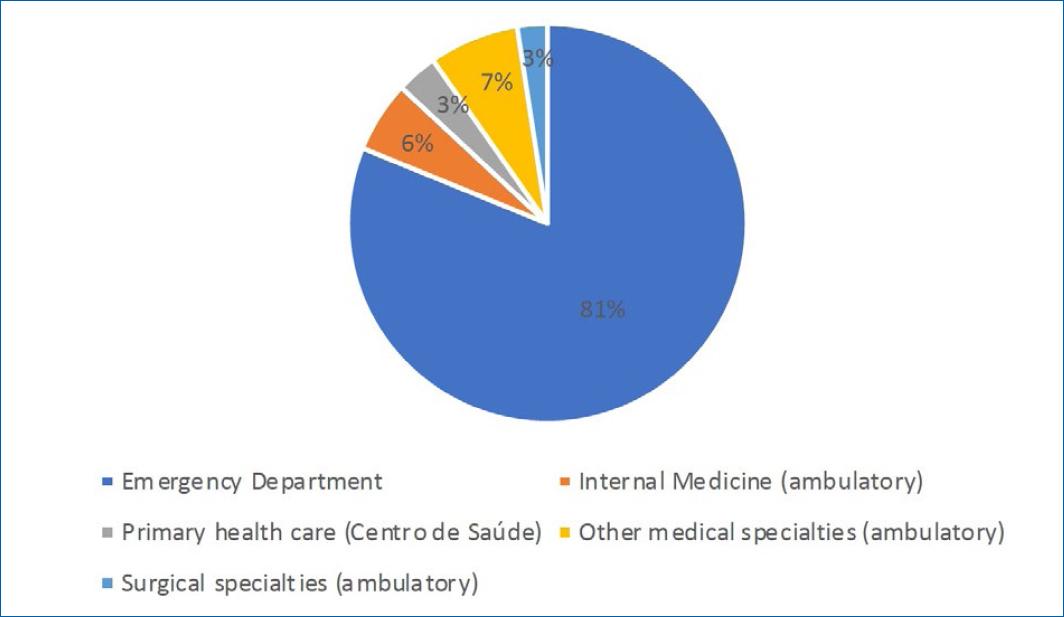
The majority of inpatient referrals originated from the Internal Medicine Wards (Fig. 3); the Emergency Department in HSJ was the most common source for urgent outpatient consultation referrals (Fig. 4).
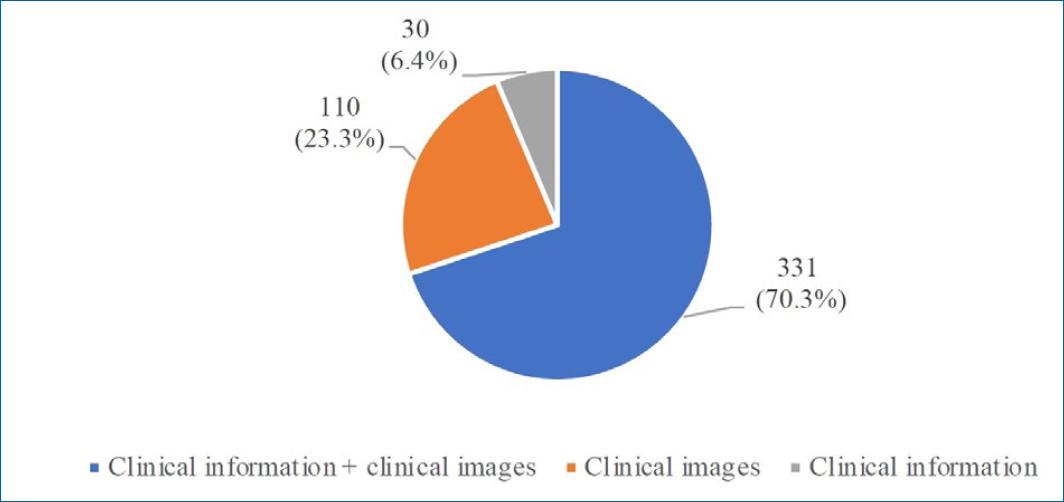
Regarding content, the majority of inpatient and outpatient referrals (331 [70.3%]) were composed of written clinical information accompanied by clinical pictures (Fig. 5); “adequat”. clinical information and clinical images were only present simultaneously in 96 cases (29%) (Table 1).
Table 1 Type of data in referrals composed of clinical information and clinical images
| Type of data | Adequate clinical Images | Inadequate clinical images |
|---|---|---|
| Adequate clinical information | 96 (29%) | 32 (9.7%) |
| Inadequate clinical information | 119 (35.9%) | 84 (25.4%) |
All other cases, composed only of written clinical information or clinical pictures, were further supplemented with additional data received by e-mail/message and/or phone calls through the Centro Hospitalar’s private network. In this subgroup, 30% and 73.64% of first received referrals were classified as containing “good qualit”. data, respectively (Table 2). Given that subsequent written information and clinical pictures were obtained after feedback from a dermatologist, this data was not evaluated in this study.
Table 2 Type of data in referrals composed of clinical information or clinical images
| Type of data | Adequate | Inadequate |
|---|---|---|
| Clinical information | 9 (30%) | 21 (70%) |
| Clinical images | 81 (73.64%) | 29 (26.36%) |
The majority of all referrals (419 [88.9%]) received a response by a dermatologist in less than 24 hours and this was also the case for subgroup analysis (Table 3). Conversion to in-person evaluation was made in 273 cases (58%), encompassing most outpatient referrals (230 [69.9%]) but less than a third of inpatient referrals. The average time for in-person evaluation after triage was 0.25 days for inpatients and 4 days for outpatients (Table 4).
Discussion
Teledermatology care can be divided into three main platforms: synchronous (real-time), asynchronous (store and forward), and mixed (a fusion of the previous two)2. The Dermatovenereology Department of HSAC implemented an asynchronous platform based on e-mail and smartphones.
These methods of communication were rapidly made available and implemented in Centro Hospitalar Lisboa Central. The e-mail was the preferred method of referral for urgent consultations; we believe that widespread availability, lack of need for specific equipment (i.e., smartphone, apps), secure integration in the hospital’s network, and the use of work credentials instead of personal ones (i.e., private phone number) contributed to this fact.
Even though these were effective means of data transfer, lack of integration with the software used throughout CHULC were a difficult challenge to overcome. The constant need of switching between software (and operative systems when it came to smartphone usage) revealed itself as time-consuming and followed a learning curve. We also believe that the ability to store clinical images into patients’ medical records (with patient consent) would be beneficial; by doing this, important clinical data would be made available to all physicians involved in a given patient’s care, regardless of medical specialty. Current storage options available at CHULC don’t grant access to this data to non-dermatologists and make future erasing of said data (due to low storage capacity, change of e-mail domains, among others) an inevitability.
Nevertheless, the successful implementation of teledermatology methods is directly impacted by the quality of the sent data. In an ideal world, only adequate clinical information and clinical pictures would be received. In this study, this was true in less than a third of referrals containing both types of data.
Without clear and detailed clinical information, the interpretation of the patient’s condition becomes difficult, making diagnosis and treatment a challenge; frequently, past medical history of patients was omitted in referrals and the evolution of the dermatosis through time was not always described. Likewise, description of past medical treatments was missing most of the time.
The absence of a clear description of dermatologic lesions was frequently found in referrals. Incorrect use of medical terms regarding primary and secondary skin lesions (especially when clinical images are lacking or inadequate), can misguide diagnosis. This problem can be addressed with adequate education of non-dermatologists regarding standard definitions of dermatological terms.
On the other hand, clinical pictures without good quality also undermine these clinical processes. Lack of focus and insufficient lighting were the most common problems identified and can be, at least partially, justified by lack of specific formation in clinical image of adequate cameras owned by the hospitals and the need to use personal cameras or taking, lack of ideal physical conditions (natural lighting for example) and time to produce adequate clinical images. Absence of adequate cameras owned by the hospitals and the need to use personal cameras or smartphones can also impact image quality.
Other difficulties arise when considering the almost 30% of cases in which referrals were only composed of clinical information or clinical pictures. This is unsatisfactory for all the previously mentioned reasons, adding up to the need of subsequent follow-ups on referrals (which increases workload not only for the dermatologist but also for the physician responsible for the referral). If this process, albeit cumbersome, can be made in inpatients referrals, its application to outpatient referrals was sometimes impossible (i.e., obtaining clinical pictures of a patient that had already left the emergency room). Evidently, one must also consider that all of this is directly reflected in delaying patient care.
It is also noteworthy the acceptance of teledermatology by patients. All patients in which the use of these methods was suggested by their physician gave their informed consent. High acceptance of COVID-19 control measures (including mobility restrictions) among Portuguese population, desire to avoid more in-person consultations and the prospect of a faster clinical response were probable drivers for this fact.
Accordingly, clinical response by a dermatologist was produced in less than 24 hours in almost 90% of all referrals, approaching almost 100% in inpatient referrals. Longer response times were associated with referrals made during the weekend or holidays (as the dermatology department only functions during working days).
Conversion to in-person evaluation was made when the clinical information and/or images were insufficient to arrive at a diagnosis, when medical or surgical procedures were necessary (as in malignant tumors) and when the complexity of the medical condition demanded it (erythrodermic patients, among others). We also consider that the average time for in-person evaluation was satisfactory.
The striking difference in conversion to in-person evaluation between inpatient and outpatient referrals can be justified, in part, by the nature of the referrals themselves. In the first case, most patients didn’t present with dermatological urgencies and were referred mostly for benign, long-term and easy to treat conditions, thus taking advantage of a hospitalization for other medical reasons for this dermatological evaluation. In contrast, a significant portion of outpatient referrals consisted of urgent or complex conditions that demanded in-person evolution, and that, in most situations, had driven the patient to an emergency room consultation in the first place.
Our study has several limitations: deleted or lost data at the time of the study couldn’t be included in this analysis and, even with pre-established criteria, the classification of “adequat”. and “inadequat”. clinical images is always observant-dependent at some level.
Arguably, the pandemic accelerated the process of implementation of new technologies to deliver better healthcare and so, even after the restrictions imposed by COVID-19 were lifted, the Dermatovenereology Department of HSAC maintained its teledermatology platforms. By allowing clinical triage and remote consultations for clinical situations where in-person evaluation is not mandatory, teledermatology made possible a faster delivery of care, while lowering work absenteeism and costs for patients and health providers.
Conclusion
The COVID-19 pandemic gave rise to a number of difficult to overcome challenges. In this particular case, the need to balance assistential activity and COVID imposed restrictions was met with the implementation and use of teledermatology methods. These were widely and rapidly accepted by physicians and patients.
During a 13-month period, the Dermatology and Venerology Department of HSAC received more than 500 referrals for inpatient and outpatient consultations, composed of clinical information and/or clinical images. A significant proportion of these was resolved remotely without the need for in-person consultation.
Insufficient clinical information in referrals, inadequate clinical images and lack of integration with clinical software were the main problems identified by this study. Its resolutions aren’t straightforward and would involve education of professionals and financial support in order to acquire new equipment and software.
Telemedicine cannot, by any means, fully replace in-person evaluation of patients and presents itself with a particular array of problems. Nevertheless, it can be a valuable work tool for professionals, especially in atypical times when all available resources must be used to assure good healthcare.