Introduction
Schistosomiasis mansoni is a systemic disease caused by a trematode helminthic which represents a public health problem in Brazil and in the world1.
Skin lesions are observed mostly in the acute phase (swimmer`s itch or cercarial dermatitis), and are very unusual in the chronic forms of schistosomiasis, even in endemic areas2.
The cutaneous form is usually asymptomatic, and it occurs often in white young women. Chronic lesions are formed when the eggs or worms migrate to the skin, causing granulomas on the skin and mucous membranes3,4.
We report the case of a male patient, who after a trip to the coast of São Paulo, developed the systemic schistosomiasis that was correctly diagnosed only after skin biopsy.
Case report
A previously healthy male patient–D.G.D., aged 17-year-old, used to swim in river waters on family trips. One month after his trip to “Juréia” and “Boracéia,” in the South Coast of São Paulo state, in February 2020, he developed fever, dry cough, and diarrhea, progressing with prostration and desaturation, requiring hospital admission and additional oxigenotherapy. With the hypothesis of viral infection (COVID-19 or Influenza), he was medicated with Oseltamivir and Amoxicillin Clavulanate, but PCR for COVID-19 and Influenza were negative.
A computed tomography (CT) of the thorax revealed multiple solid sparse nodules distributed bilaterally on the lung parenchyma, some of them with halo in opaque glass, measuring up to 10 mm, and additional splenomegaly. Laboratory examinations showed leucocytosis (15.090/mm3) with 38.2% eosinophils (5.760/mm3). A protoparasitological examination of feces was negative. Pneumonology suspected of Löffler`s Syndrome, and prescribed Ivermectin 18 mg/day for 2 days and Albendozole 400 mg/day for 6 days, aiming to treat Ascaris lumbricoides or Strongyloides stercoralis. Nevertheless, one day after onset of this treatment, he developed a cutaneous rash on the dorsum, axillae and inguinal region (Fig. 1), suggesting possible toxemia secondary to antigen release from the dead helminths. Hydrocortisone 100 mg every 12 hours was soon initiated with improvement of the rash in a few days.

Figure 1 A and B: maculopapular exanthema with predominant involvement of the axillae (A), inguinal region and dorsum (B), which developed within 24hours on onset of Albendazole and Ivermectin.
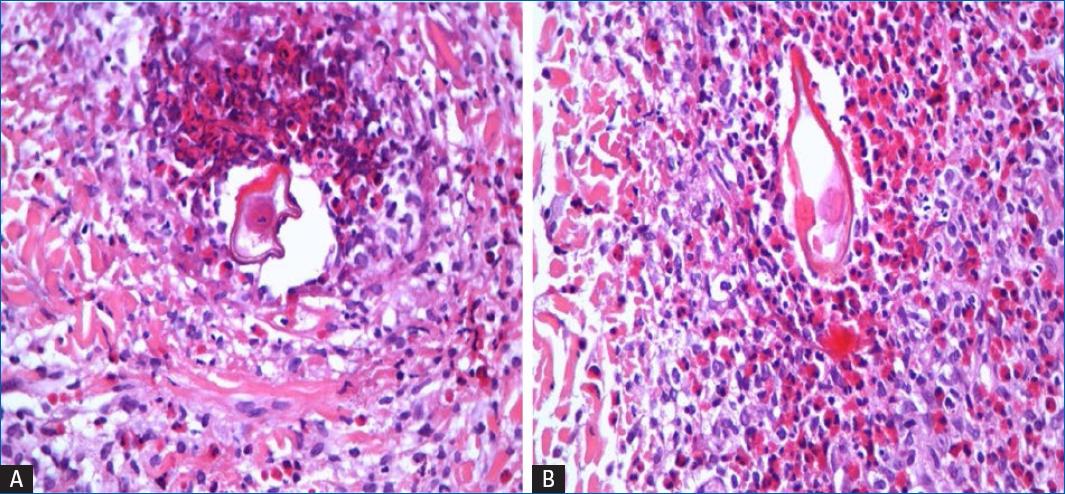
However, just 2 days after stopping Ivermectin, the patient developed symmetrical erythematous papular lesions, some isolated and with minor excoriations and others confluent into small plaques, localized on the buttocks and perianal area (Fig. 2). A skin biopsy of the right buttock demonstrated eosinophilic granulomas associated with typical parasitic eggs (Fig. 3), confirming the diagnosis of Schistosomiasis. Also indirect immunofluorescence assay to S. mansoni was positive 1/64. Treatment with praziquantel, 4.2 g as a single dose induced total relief, improving his clinical status after 1 week, including complete resolution of perianal cutaneous lesions.
Discussion
Schistosomiasis is still a serious health problem in Brazil6, with S. mansoni as the only species found in this country8. It is acquired in contact with contaminated water, and transmission depends on snails of the genus Biomphalaria, found in freshwater-bathed regions7. When carrying out their domestic and leisure activities in rivers, lakes and ponds, humans are exposed to the larva, that have left the snails, which actively penetrate the skin and mucous membranes7. The larvae reach the blood vessels and portal circulation, where they will become adult worms8.
Soon, after the infective contact, cercarial dermatitis may occur, which presents with pruritus, usually transient, and an erythematous micropapular eruption. After about 40-60 days, coincident with the laying of eggs6, usually in the mucosa and submucosa of the colon and rectum veins9, patients develop high fever, chills, sweating, malaise and asthenia, followed by diarrhea, nausea, and vomiting, which constitute the phase entitled Katayama fever. Associated hepatosplenomegaly and significant eosinophilia, often lead to the diagnosis of acute schistosomiasis7. In its chronic phase that occurs more than 6 months after infection various organs may be affected with signs and symptoms of intestinal, hepato-intestinal or hepatosplenic involvement, as well as neurological and cutaneous forms7,8. Tissue granulomas may form in response to the presence of the eggs, classically leading to bowel wall thickening, periportal fibrosis of the liver and portal or pulmonary hypertension10.
Pulmonary involvement can be divided into two vascular clinical forms: hypertensive and cyanotic. The first is characterized by dyspnea on exertion, palpitations, dry cough, and constrictive chest pain, which can also lead to extreme asthenia and fatigue, in addition to heart failure. The cyanotic form has a worse prognosis and presents with generally mild cyanosis, especially in the extremities6. Pulmonary manifestations can also occur during the migration of larval forms, such as the so-called Loffler syndrome, manifesting with dyspnea and dry cough and characterized by accumulation of eosinophils in the lungs10, which is consistent with the initial presentation of the present case that did not show the typical signs of Katayama fever.
Skin lesions of chronic schistosomiasis are generally characterized as papular, ulcerative, granulomatous, and fistulous lesions, often affecting the skin of the genital and perianal region, secondary to the deposition of eggs contiguous to the pelvic vessels9. Infiltrative lesions in these regions can cause an inflammatory and fibrotic reaction, leading to the formation of granulomas that begin as asymptomatic firm papules that grow slowly, until they become vegetative8. In rare circumstances, the eggs are lodged in extragenital skin, causing cutaneous ectopic schistosomiasis9, and lesions may be found on the back and abdomen. The exact mechanism of egg deposition in the skin remains unknown, suggesting that anastomoses between venous systems would be associated with the migration of eggs or adult worms to ectopic sites8.
Diagnosis is based on characteristic lesions, compatible epidemiology and histopathological examination3. Histopathology provides identification of S. mansoni eggs, surrounded by inflammatory cells, mainly lymphocytes and eosinophils in more recent lesions, but in old lesions necrosis and granulomatous infiltrates predominate2,10. The coprologic examination can be used preferably with the use of quantitative and sedimentation techniques4. Diagnosis can also be confirmed by combining the results of an indirect hemagglutination assay and enzyme-linked immunosorbent assay test, which reach a sensitivity and specificity beyond 90 and 97% respectively5. As in our case significant eosinophilia is very frequent. Meltzer et al. described that 53.7% if patients with significant eosinophilia after a trip were diagnosed with schistosomiasis. Around 47.7% of the patients suffered from schistosomiasis acute crisis, 16.9% patients presented chronic symptoms and 36.6% were asymptomatic5.
The gold standard treatment is praziquantel 60 mg/kg for children until 15 years old and 50 mg/kg for adults, in a single dose with high healing rates (60-90% in endemic areas and about 100% in non-endemic areas)2,10. The second-choice drug is the oxamniquine 15 mg/kg, a single dose in adults, and 20 mg/kg, as single dose on children up to 15 years old.
What does this study add to the current knowledge?
This study approaches a rare case of cutaneous schistosomiasis with Löffer syndrome, a rare presentation, despite being an endemic disease in Brazil. We`ve alerted to the necessity for the accurate diagnosis, which in this case was based on the skin biopsy.