Case report
A 61-year-old man skin type II presented to our outpatient clinic with a suspicious lesion within a tattoo on his right upper arm for an unknown period of time. On examination, he had a soft, sharply demarcated bluish papule measuring 7 mm with a smooth surface. The papule could be pressed into the level of the skin. Incident light microscopy revealed blue lacunae outside the tattoo and blackish structureless portions in the area of the overlying tattoo (Fig. 1, black arrow). In addition, distal to the lesion described above, he had a symmetrical, irregularly pigmented, and approximately 5 mm in diameter brown macule. Incident light microscopy revealed an irregular internal structure consisting of reticular lines and clods with questionable heterochromia. The assessability to this lesion was considerably limited by the tattooing (Fig. 1, red arrow).

Figure 1 Two pigmented lesions over a black tattoo whose histopathology revealed an hemangioma (black arrow) and a melanoma explanation only in text (not beneath photo).
The patient’s past medical history included diabetes mellitus, arterial hypertension, attention deficit hyperactivity disorder, benign prostatic hyperplasia, and fibromyalgia. He also reported a history of melanoma that had been excised from the back about 30 years earlier. The tumor data could no longer be obtained. Furthermore, a superficial spreading melanoma on the right thigh (tumor thickness 0.5 mm, Clark level II, < 1 mitosis/ mm2, no nevus association) had been excised in our clinic 2 years prior. Both melanomas had occurred in non-tattooed skin. Follow-ups with a dermatologist had always been unremarkable. As a child, the patient suffered several sunburns.
The two lesions described above were excised under local anesthesia. Histology of the proximal lesion revealed a hemangioma (Fig.1, black arrow), and of the distal lesion (Fig.1, red arrow) a superficial spreading melanoma in the tattoo (Fig. 2 and 3), Clark level II, vertical tumor thickness- Breslow 0.3 mm (pT1a). There was no ulceration or regression.
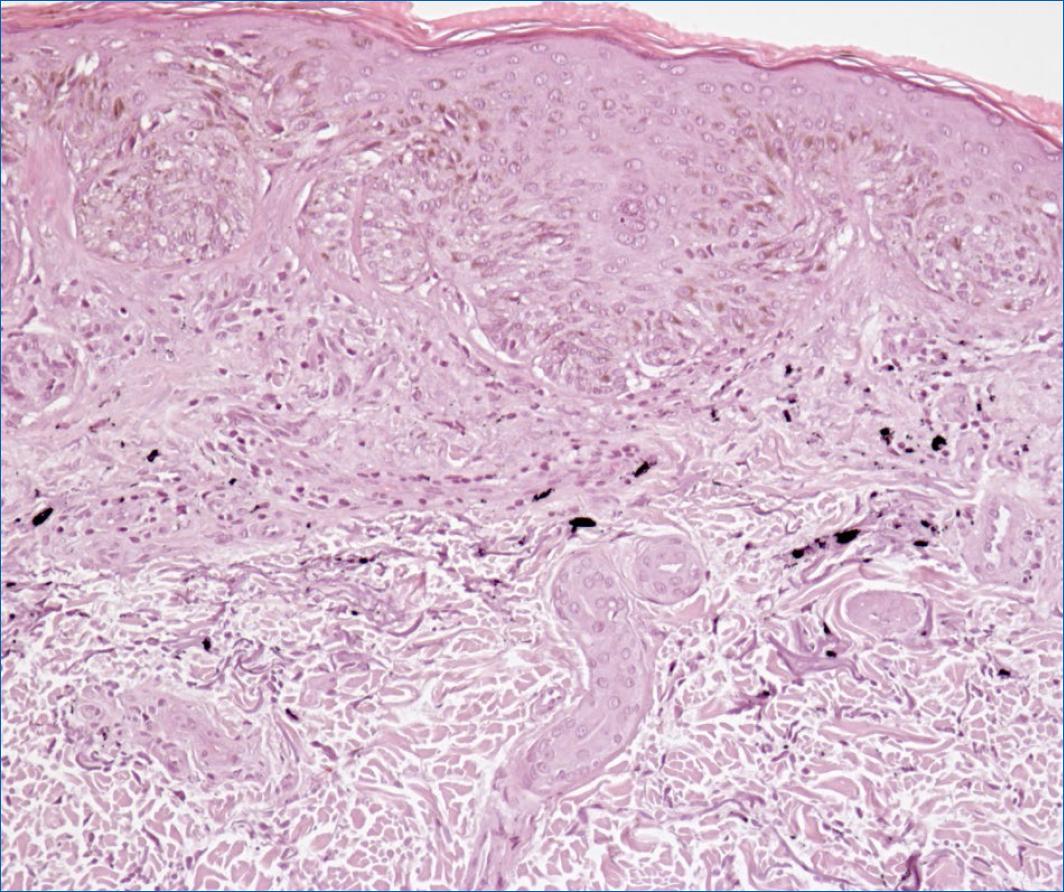
Figure 2 Irregular melanocytic proliferation with formation of nests of atypical melanocytes in the area of the junctional zone and in the adjacent corium. Proliferation of single atypical melanocytes in the basal cell layer with suprabasal storage, discharge into the stratum corneum. Inhomogeneous pigment incontinence and moderate inflammatory infiltrates. In addition, granular to scaly pigment deposits are found in the upper to middle corium. Also, solar elastosis. Diagnosis: superficial spreading melanoma in tattoo, Clark level II, vertical tumor thickness according to Breslow 0.3 mm, (pT1a). No ulceration. No regression. No nevus association.
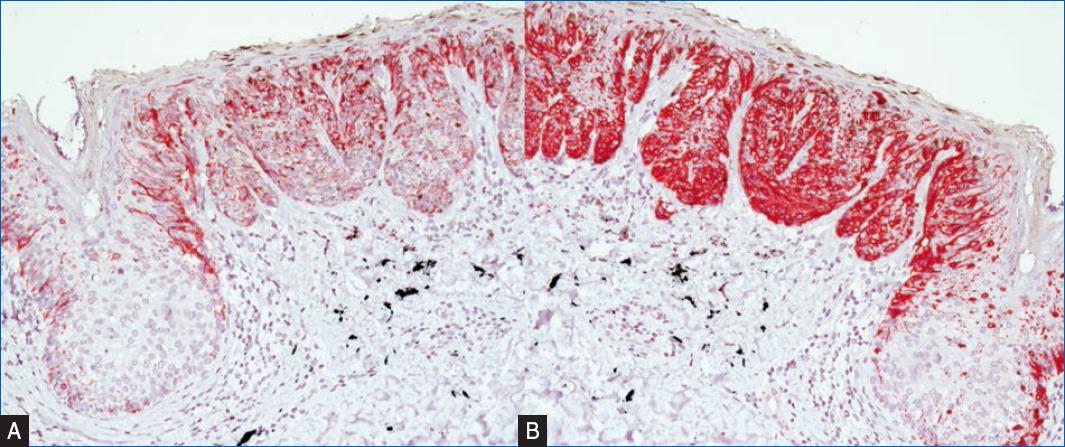
Figure 3 Immunostaining Melan A and HMB45. A: immunostaining with monoclonal anti-MART-1/MelanA-antibody (200x) MelanA-Staining marks melanocytes in all layers of the epidermis. B: immunostaining with monoclonal anti-HumanMelanomaBlack (HMB45)—antibody (200x) HMB45-Stainings marks premelanosome protein (PMEL) in proliferating melanocytes in all layers of the epidermis.
Discussion
In the present case, tattooing occurred in the history of two malignant melanomas. A third melanoma developed in the black tattoo, which significantly complicated the diagnosis of the third melanoma during tumor follow-up, although we were still able to diagnose and remove the melanoma while it was in stage I. With already two pre-existing melanomas, skin metastasis can also be considered. These often appear to be dark, red, or skin-colored papules or nodules.
We interpret the hemangioma as incidental.
Early detection of malignant melanoma with the aim of excision at low tumor stages is a major goal of dermatologic screening. The rising incidence of melanoma in Germany is currently reported to be 26.5 cases (men) and 25.3 cases (women) per 100,000 inhabitants per year. For tattoos, a prevalence of 14% in Western countries and up to 50% among 25-35-year-olds are reported1-5. With the increasing incidence of melanoma coupled with the increasing prevalence of tattoos, a cumulative occurrence of melanoma in tattooed individuals must be expected.
To our knowledge, 36 cases of melanoma in tattoos have been reported in the literature to date. The risk for melanoma development does not appear to be increased per se in tattooed skin6,7. But morphologic evaluation is complicated by the exogenous pigment, resulting in a possible delay in diagnosis8. Suspicious nevi can be covered by tattoos so evaluating the nevi is extremely difficult at the clinical and dermoscopic levels. In addition to the generally more difficult assessability, especially dermal signs of malignancy, such as blue or gray veils, can be disguised by a tattoo. Therefore, tattooing must be viewed extremely critically in the presence of multiple and/or atypical nevi syndrome and melanoma in the patient’s own and/or family history.
In addition, a thorough dermatologic examination should be performed prior to any laser therapy of a tattoo to avoid triggering changes in nevi or melanoma-specific lesions9,10,11. If laser therapy is specifically desired and indicated, we recommend excising pigmented lesions in the tattoo prior to laser therapy and submitting them to histologic examination. Regarding carcinogenic ingredients of tattooing products, a negative list exists in Germany since 2009, though it has not been established if avoiding these ingredients decreases malignancy risk12. In addition to the usual provisos, UV protection in the area of tattoos is recommended since UV radiation can potentially alter tattoo ingredients and lighten the tattoo under UV irradiation13-15.
Summary and conclusion
There should be a low threshold for performing biopsies in suspicious melanocytic lesions within a tattoo, as morphologic malignancy criteria may be obscured by the exogenous pigment.
Tattoos should be very carefully considered in people with multiple nevi syndrome, atypical nevi, and a history of melanoma in self and/or family. No tattoo should be applied in the area of nevi. People with this history should see a dermatologist prior to obtaining a tattoo and obtain regular skin checks after.
Although no correlation between melanoma development and tattooing has been found from the literature available to date, extreme caution should be exercised with tattooing in patients at increased risk for melanoma and prior to laser therapy.














