Introduction
Skin diseases represent about 30% of pediatric consultations in health systems, with high prevalence in different levels of health care1-4. These conditions can have a great psychological and social impact on the affected individuals, impairing their quality of life and daily activities, especially in the pediatric population, which is more sensitive and vulnerable5.
Dermatological disorders may present as primary cutaneous diseases, acute or chronic, as well as secondary manifestations of systemic conditions, which may exacerbate or spread, causing associated complications that can be life-threatening6-8. Thus, due to the potential risk to life, especially for children and adolescents, such clinical conditions may require hospitalization, being initially managed by pediatric hospital teams6-8.
Considering the particularities of skin manifestations in children and adolescent populations, pediatricians may demonstrate a certain degree of difficulty with their diagnosis and treatment2,9,10. Hence, dermatology can offer important contributions to inpatient care, providing backing to the management of pediatric patients by performing hospital consultations11.
Thus, in view of the relevance of dermatology in hospital settings, it is pertinent to comprehend the profile of dermatologic consultations, identifying clinical practices, diagnostic and therapeutic patterns, as well as contributions to pediatric services. Therefore, this study aimed to analyze the profile of pediatric consultations performed by a dermatology service in a hospital complex in Southern Brazil.
Method
This descriptive and quantitative study was conducted from the analysis of admissions, hospital referrals, and dermatology consultations of inpatients admitted to Hospital da Criança Santo Antônio, the pediatric segment of the hospital complex Santa Casa de Misericordia de Porto Alegre, in Southern Brazil. The research was approved by the Human Research Ethics Committee of the institution and included hospitalization data from 1st August 2018 to 31st January 2020.
From a preliminary data collection, we identified 12,656 pediatric hospitalizations and 816 consultation referrals forwarded to the dermatology Service. Subs-equently, we carried out an exploratory analysis, which excluded suspended requests and duplicate referrals from the same medical speciality. Posteriorly, we proceeded to an investigation organized into three analytical phases: analysis of pediatric hospitalizations with dermatological diagnosis (phase 1), analysis of dermatology consultations referrals (phase 2), and analysis of dermatology consultations (phase 3). It is worth mentioning that, based on the analysis of consultations referrals, we performed an additional exclusion procedure of duplicate referrals, even those from different specialties, in order to proceed with the analysis of dermatology consultations.
Considering this research arrangement, we analyzed three groups of variables: “pediatric skin diseases”, reported by inpatient pediatric teams; “profile of consultations referrals” (hospital sector, pediatric subspecialties, patients’ age and sex, clinical data, and diagnostic hypotheses) and “profile of dermatology consultations” (clinical description, complementary exams, dermatological diagnoses, therapeutic conducts, and recommend follow-ups).
Regarding consultation referrals, according to W Huang and Chong S12, we established four analysis parameters: “morphology of skin lesions,” “distribution of skin lesions,” “evolution of clinical condition,” and “diagnostic hypothesis or purpose of referral.” Dermatological diagnoses were established according to the International Classification of Diseases (ICD-10).
With respect to follow-up recommendations, we considered “outpatient follow-up” for those hospital consultations whose duration of dermatology assistance was equal to or < 7 days, followed by recommendations for outpatient follow-up. In contrast, “inpatient + outpatient follow-up” were considered hospital consultations whose dermatology assistance duration was longer than 7 days, with a recommendation for outpatient follow-up after completion.
In statistical analysis, categorical and numerical variables were represented descriptively by measures of dispersion and frequencies, whereas the groups of hospital dermatoses were analyzed by chi-squared test (X2), considering p-value ≤ 5% statistically significant.
Results
Dermatological hospitalizations and consultations referrals
During the period of August 2018-January 2020, we identified 12,656 pediatric hospitalizations, with 865 dermatological ICDs registered, which represents 6.8% of the total hospitalizations. The main dermatological ICDs were “cellulitis and acute lymphangitis” (14.3%), “cutaneous abscess, furuncle, and carbuncle” (11.0%), and “purpura” (8.8%) (Table 1).
Table 1 Pediatric hospital dermatoses and dermatological consultations referrals
| n | % | |
|---|---|---|
| Pediatric hospitalizations | 12.656 | 100.0 |
| ICD diagnosis of skin diseases among pediatric hospitalizations | 865 | 6.8 |
| Referrals for dermatological consultations | 266 | 2.1 |
| Dermatological consultations | 167 | 1.3 |
| Major skin diseases ICDs | ||
| L03-Cellulitis and acute lymphangitis | 124 | 14.3 |
| L02-Cutaneous abscess. furuncle and carbuncle | 95 | 11.0 |
| D69-Purpura | 76 | 8.8 |
| L50-Urticaria | 56 | 6.5 |
| L90-Atrophic disorders of skin | 47 | 5.4 |
| L98-Other disorders of skin and subcutaneous tissue | 44 | 5.1 |
| L01-Impetigo | 31 | 3.6 |
| L20-Atopic dermatitis | 31 | 3.6 |
| L72-Follicular cysts | 30 | 3.5 |
| D18-Hemangioma and vascular malformations | 29 | 3.4 |
Dermatology referrals included 266 referrals from hospital teams, either from the pediatric ward (54.5%) or the pediatric emergency (37.6%) as the main requesting hospital sectors. Most of the referrals originated from general pediatrics (73.3%) and pediatric oncology (8.3%). The majority of pediatric patients were hospitalized under public health system coverage (66.1%) (Table 2).
Table 2 Profile of hospital dermatological consultations referrals
| n | % | |
|---|---|---|
| Hospital sector | ||
| Pediatric ward | 145 | 54.5 |
| Pediatric intensive care unit | 17 | 6.4 |
| Pediatric emergence | 100 | 37.6 |
| Pediatric surgery unit | 4 | 1.5 |
| Sector character | ||
| Public health system | 176 | 66.1 |
| Private health system | 69 | 25.9 |
| Mixed | 21 | 7.9 |
| Pediatric subspecialties | ||
| General pediatrics | 195 | 73.3 |
| Intensive pediatrics | 9 | 3.4 |
| Pediatric endocrinology | 1 | 0.4 |
| Pediatric gastroenterology | 4 | 1.5 |
| Pediatric hematology | 8 | 3.0 |
| Pediatric infectology | 11 | 4.1 |
| Pediatric oncology | 22 | 8.3 |
| Pediatric pneumology | 3 | 1.1 |
| Pediatric nephrology | 5 | 1.9 |
| Pediatric neurology/neurosurgery | 6 | 2.2 |
| Pediatric surgery | 1 | 0.4 |
| Neonatology | 1 | 0.4 |
| Clinical information on referrals | ||
| No variable described | 129 | 48.5 |
| 1 variable described | 54 | 20.3 |
| 2 variables described | 49 | 18.4 |
| 3 variables described | 24 | 9.0 |
| 4 variables described | 10 | 3.7 |
| Description of skin lesions | 56 | 21.0 |
| Location of skin lesions | 80 | 30.0 |
| Time of clinical evolution | 22 | 8.3 |
| Diagnostic hypothesis | 74 | 27.8 |
| Referral status | ||
| Consultation performed | 167 | 62.8 |
| Duplicate referral | 53 | 19.9 |
| Suspended or lost referral | 46 | 17.3 |
| Total | 266 | 100.0 |
In relation to referrals’ information, a significant portion of them did not present data about clinical conditions (48.5%). The location of skin lesions was the most referred clinical data (30.0%). Only 3.7% of referrals reported the four clinical parameters analyzed, whereas diagnostic hypotheses were indicated in only 28.5% of the dermatology referrals (Table 2).
Profile of dermatology consultations
After preliminary analysis and duplicate referrals exclusion, we identified 167 pediatric consultations performed by the dermatology team during the 18-month period, with a response time of < 24 hours for most of the evaluations (80%). Most inpatients were males (56.9%), “younger than 1 year” (19.2%), or “11-14 years” (19.2%). Most evaluations led to single diagnoses (77.8%), with “dermatitis and eczema” and “skin infections” standing out as the most prominent groups of dermatoses, with 38.7 and 31.2%, respectively (Table 3).
Table 3 Profile of hospital dermatological consultations
| Total | 167 consultations | ||
| Monthly average | 9.3 consultations | ||
| Daily average | 0.3 consultations | ||
| n | % | ||
| Hospital sector | |||
| Pediatric ward | 87 | 52.1 | |
| Pediatric intensive care unit | 6 | 3.6 | |
| Pediatric emergence | 73 | 43.7 | |
| Pediatric surgery unit | 1 | 0.6 | |
| Patient demographics | |||
| Gender | |||
| Male | 95 | 56.9 | |
| Female | 72 | 43.1 | |
| Age group* | |||
| Neonates | 16 | 9.6 | |
| Infants | 16 | 9.6 | |
| Toddlers | 23 | 13.8 | |
| Preschoolers | 27 | 16.2 | |
| Schoolers | 29 | 17.4 | |
| Adolescents | 56 | 33.6 | |
| Dermatological diagnoses** | |||
| One diagnosis | 130 | 77.8 | |
| Two diagnoses | 30 | 18.0 | |
| Three diagnoses | 3 | 1.8 | |
| Complementary exams*** | |||
| Skin biopsy | 18 | 10.8 | |
| Bacterial culture | 10 | 6.0 | |
| Direct mycological examination | 9 | 5.4 | |
| Tzanck’s smash | 3 | 1.8 | |
| Imaging exams | 8 | 4.8 | |
| Laboratory exams | 49 | 29.3 | |
| Therapeutic recommendations | |||
| Antibiotics | |||
| Yes | 38 | 22.7 | |
| Topical | 5 | 3.0 | |
| Systemic | 33 | 19.7 | |
| No | 129 | 77.3 | |
| Corticosteroids | |||
| Yes | 59 | 35.3 | |
| Topical | 35 | 20.9 | |
| Systemic | 24 | 14.4 | |
| No | 108 | 64.7 | |
| Antifungals | |||
| Yes | 10 | 6.0 | |
| Topical | 7 | 4.2 | |
| Systemic | 3 | 1.8 | |
| No | 157 | 94.0 | |
| n | % | ||
| Antiviral | |||
| Yes | 6 | 3.6 | |
| Oral acyclovir | 3 | 1.8 | |
| Intravenous acyclovir | 3 | 1.8 | |
| Other antivirals | 0 | 0.0 | |
| No | 161 | 96.4 | |
| Antiparasitic* | |||
| Yes | 19 | 11.4 | |
| Permethrin | 1 | 0.6 | |
| Ivermectin | 4 | 2.4 | |
| Permethrin + ivermectin | 7 | 4.2 | |
| Sulfur 6% | 7 | 4.2 | |
| No | 148 | 88.6 | |
| Moisturizer | |||
| Yes | 44 | 26.3 | |
| Specific | 23 | 13.8 | |
| Generic | 21 | 12.5 | |
| No | 123 | 73.7 | |
| Total | 167 | 100.0 | |
*Age groups: neonates (under 1 month); infants (2-11 months); toddlers (1-2 years); preschoolers (3-5 years); schoolers (6-10 years); adolescents (11-17 years).
**Due to the multiple diagnoses, the total of 167 consultations corresponds to 199 dermatological diagnoses.
***Multiple response variables.
Regarding the profile of dermatoses by age groups, we observed a higher prevalence of “Skin infections” among neonates, infants, and preschoolers, whereas “dermatitis and eczema” were most frequent among schoolers and adolescents (Figure 1). About dermatological ICDs, “scabies” (B86) and “impetigo” (L01) stood out among the major skin diseases at younger ages, whereas “drug eruptions” (L27) were more relevant with advancing age, particularly in adolescence. “Atopic dermatitis” (L20) exhibited high prevalence in all age groups but with greater expression in preschoolers and schoolers (Table 4).
Table 4 Major diagnostic ICDs of dermatological consultations by age groups
| n | % | ||
|---|---|---|---|
| L20-atopic dermatitis | 32 | 23.7 | |
| L27-drug eruptions | 23 | 17.0 | |
| L01-impetigo | 18 | 13.3 | |
| B86-scabies | 17 | 12.6 | |
| L70-acne | 10 | 7.4 | |
| L21-seborrheic dermatitis | 10 | 7.4 | |
| B00-herpesvirus infections | 9 | 6.7 | |
| L50-urticaria | 6 | 4.4 | |
| L30-unspecified dermatitis | 6 | 4.4 | |
| Q89-congenital malformations | 4 | 3.0 | |
| ICDs of dermatological consultations | |||
| Neonates Under 1 month | L21-seborrheic dermatitis | 8 | 27.6 |
| B86-scabies | 6 | 20.7 | |
| L01-impetigo | 4 | 13.8 | |
| L20-atopic dermatitis | 4 | 13.8 | |
| B081-molluscum contagiosum | 1 | 3.4 | |
| Infants 2-11 months | B86-scabies | 2 | 15.4 |
| L20-stopic dermatitis | 2 | 15.4 | |
| B00-herpesviral infections | 1 | 7.7 | |
| B87-myiasis | 1 | 7.7 | |
| D18-hemangioma and lymphangioma | 1 | 7.7 | |
| Toddlers 1-2 years | B86-scabies | 5 | 17.2 |
| L01-impetigo | 3 | 10.3 | |
| B081-molluscum contagiosum | 2 | 6.9 | |
| L20-atopic dermatitis | 2 | 6.9 | |
| L53-other erythematous conditions | 2 | 6.9 | |
| Preschoolers 3-5 years | L20-atopic dermatitis | 6 | 18.2 |
| L27-drug eruptions | 4 | 12.1 | |
| L01-impetigo | 3 | 9.1 | |
| L50-urticaria | 3 | 9.1 | |
| B00-herpesviral infections | 2 | 6.1 | |
| Schoolers 6-10 years | L20-atopic dermatitis | 10 | 30.3 |
| L01-impetigo | 4 | 12.1 | |
| L27-drug eruptions | 4 | 12.1 | |
| L30-unspecified dermatitis | 2 | 6.1 | |
| L40-psoriasis | 2 | 6.1 | |
| Adolescents 11-17 years | L27-drug eruptions | 13 | 19.7 |
| L20-atopic dermatitis | 8 | 12.1 | |
| L70-acne | 8 | 12.1 | |
| B00-herpesviral infections | 6 | 9.1 | |
| L01-impetigo | 3 | 4.5 | |
*International Classification of Diseases (ICD-10).

Figure 1 Groups of skin diseases in dermatological consultations, by age groups*. *Total of 167 consultations corresponds to 199 dermatological diagnoses; chi-square test 63,502, p = 0,029. **Age groups: neonates (under 1 month); infants (2-11 months); toddlers (1-2 years); preschoolers (3-5 years); schoolers (6-10 years); adolescents (11-17 years). ***Infectious dermatoses and ICDs: bacterial infections (L00, L01, L02, L03, L08, A30, A46, A53); viral infections (B00, B01, B02, B07, B08, B97); fungal infections (B35, B36, B37, B42); parasitic infections and infestations (B85, B86, B87).
Laboratory tests (29.3%) and skin biopsies (10.8%) were the main requested complementary exams. Skin biopsies presented anatomopathological reports in concordance with the clinical diagnoses of dermatology teams in 66.6% of the evaluations (n = 12/18). “Bacterial cultures” were requested only in 6% (n = 10/167) of hospital consultations, with Staphylococcus aureus as the most prevalent etiologic agent (40%; n = 4/10).
With respect to dermatologists’ management, corticoids were the most recommended drugs in consultations (35.7%), with a predominance of topical presentations (59.3%), followed by moisturizers (26.3%) (Table 3). Antibiotics were indicated in 22.7% of the dermatology evaluations, highlighting the systemic presentation (n = 33/86.8%), mainly oxacillin (n = 14/38; 36.8%) and cephalexin (n = 9/38; 23.7%).
“Outpatient follow-up” and “inpatient and outpatient follow-up” were the leading orientations of dermatology follow-up, appearing in 35 and 32% of hospital consultations, respectively. Furthermore, 4.8% (n = 8/167) of dermatological consultations presented loss of follow-up during the dermatology hospital assistance, whereas 28.7% (n = 48/167) were managed and discharged by the dermatology team without the need for additional outpatient follow-up (Figure 2).
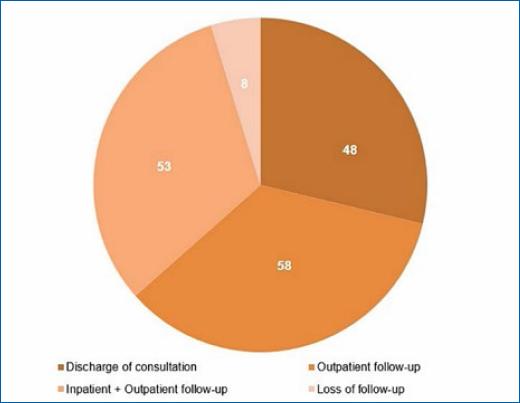
Figure 2 Follow-up recommendations of dermatology consultations*. *Outpatient follow-up’ consists of dermatological consultations whose duration of dermatology assistance was ≥ 7 days and with recommendation for outpatient follow-up after completion. “Inpatient + outpatient follow-up” included dermatological consultations whose dermatology assistance duration was longer than 7 days and with a recommendation for outpatient follow-up after completion.
Discussion
Although dermatology reveals an essentially outpatient character, the speciality provides significant contributions to the management of skin diseases in hospital settings, both for adult and pediatric patients10,13. From this perspective, our findings evidenced the relevance of hospital dermatoses in a pediatric population, representing 6.8% of hospital diagnoses, in line with a similar American study, which pointed out a prevalence of 4.2%14. Thus, proper management of these cutaneous conditions is essential to prevent complications and poor prognosis.
In contrast, hospital dermatoses are commonly assisted by non-dermatologists’ teams, which often do not properly diagnose these clinical conditions. In view of this tendency, dermatology consultations figure as a meaningful resource to support the assistant medical teams9. From our findings, we identified 266 pediatric referrals to dermatology, most of them coming from “general pediatrics” and from pediatric wards and emergency sectors, as noted in previous studies2,4,10.
In the pediatric population, likewise in adults, hospital dermatoses often manifest as acute or life-threatening conditions, entering hospitals through emergency services. According to Alba-Rojas EL et al.15, skin disorders are among the ten most common classes of diseases in pediatric emergencies. In accordance with such authors, we observed 37.6% of dermatology consultation referrals originated from the emergency department, a higher prevalence than in other studies in India4,10 and Turkey2.
Regarding consultation referrals, despite the relevance of clinical information for the efficient support of consultant teams, about half of referrals to Dermatology did not present any clinical data, which may suggest a certain difficulty for pediatricians in skin disorders management. On the other hand, in referrals with clinical information, the location of cutaneous lesions was the most reported data, although, in most of them, few features were mentioned. Inconsistencies in hospital referrals to Dermatology were also identified by Daye M et al.2, from a study in a Turkish institution.
In view of these findings, we highlighted the relevance of adequate teaching of dermatology throughout the medical course, mainly in an internship, providing the development of clinical and examination skills in the approach to skin diseases.
Dermatology consultations: epidemiology of hospital skin diseases
Throughout the 18-month period analyzed, dermatology teams performed 167 hospital consultations, with a higher prevalence of adolescent and schooler inpatients, converging with a study in a Brazilian university hospital16. Conversely, this trend differs from findings in a Turkish pediatric hospital, where infants and preschool were the most frequent age groups9.
These contrasts can be related to demographic and epidemiological differences between the populations of such countries or even reflect methodological divergences insofar as studies with pediatric populations tend to adopt different compositions of age groups, hampering comparative analysis. Thus, if we consider age, one-third of dermatology consultations addressed 2-year-old or younger patients, which may represent an immunological immaturity and a higher life-threatening risk in the early stages of life9.
Regarding the profile of dermatoses, the main groups of diagnoses were “dermatitis and eczema” and “skin infections”, agreeing with previous investigations2,4,10,17 (Table 5). Hence, “drug eruptions” (L27) and “atopic dermatitis” (L20) figured as the most prevalent cutaneous disorders assisted by dermatology consultations, followed by “impetigo” (L01) and “herpes virus infections” (B00), which were the most frequent skin infections.
Table 5 Literature review about Pediatric Hospital Dermatology
| Author (year) | Institution | City (Country) | Duration | Period of time | Casuistry | Main groups of skin diseases (%) |
|---|---|---|---|---|---|---|
| Ferreira et al. (Present study) | Federal University of Health Sciences of Porto Alegre / Santa Casa de Misericordia de Porto Alegre | Porto Alegre (Brazil) | 18 months | August, 2018- January, 2020 | 167 patients | Dermatitis and eczema (38.7) Skin infections (31.5) Disorders of skin appendages (10.5) |
| Garg et al.4 * (2019) | Lady Hardinge Medical College and Associated Hospitals | New Delhi (India) | 17 months | November, 2015-March, 2017 | 525 patients | Skin infections (58.6) Eczema (17.6) Urticaria (8.3) |
| Srinivas et al.10 (2015) | Indira Gandhi Institute of Child Health | Bangalore (India) | 42 months | January, 2010-June, 2013 | 486 patients | Skin infections (23.7) Genodermatoses (11.9) Drug reactions (8.0) |
| McMahon et al.16 (2013) | Children’s Hospital of Philadelphia | Philadelphia (USA) | 52 months | January, 2006-April, 2010 | 427 patients | Miscellaneous (41.0) Skin infections (19.0) Dermatitis (15.7) |
| Afsar9 (2017) | Dr. Behcet Uz Children’s Hospital | Izmir (Türkiye) | 76 months | January, 2004-April, 2010 | 539 patients | Allergic skin diseases (47.1) Skin infections (14.7) Systemic disorders with skin manifestations (10.2) |
| Peñate et al.18 (2012) | Hospital Universitario Insular de Gran Canaria | Las Palmas de Gran Canaria (Spain) | 10 years | January, 2000- January, 2009 | 387 patients | Inflammatory skin diseases (38.5) Skin infections (18.3) Congenital anomalies (6.9) |
| Daye et al.2 (2019) | Necmettin Erbakan University Meram Medical Faculty | Konya (Türkiye) | 1 year | September, 2016- September, 2017 | 628 patients | Skin infections (32.1) Eczema (28.2) Miscellaneous (21.5) |
*The authors included outpatients and inpatients in the study casuistry.
Atopic dermatitis is one of the most frequent dermatological causes of pediatric hospitalizations, particularly in preschool and school ages1,2,9,18,19. This condition may evolve with recurrent exacerbations, presenting eczema, erythroderma, and secondary infections, then requiring hospital care1,20. With this in mind, the high prevalence of atopic dermatitis and skin infections can suggest their concomitance, as asserted by Narla S and Silverberg JI20, who pointed out the greater susceptibility to bacterial and viral infections among patients with atopic dermatitis. According to Storan ER et al.18, timely pediatric hospitalizations can contribute both to managing atopic dermatitis, as well as to support parents and caregivers in the adherence to medical and non-medication measures for controlling the disease. Nonetheless, on the other hand, hospital environments may also represent health risks, mainly due to recurrent administration of medications and exposure to nosocomial bacteria.
During the hospital stay, medications are often necessary and widely prescribed by assistant teams, especially in systemic forms. However, the administration of multiple drugs, along with debilitated patients’ conditions, increases the risk of drug reactions2. Drug reactions can induce a broad range of clinical manifestations, which often involve the skin, namely morbilliform exanthema, Stevens-Johnson syndrome, toxic epidermal necrolysis, among others10. Corroborating this perspective, we observed a high prevalence of drug eruptions among pediatric inpatients, particularly in the adolescent group.
Furthermore, the skin fragility of early pediatric age groups also increases the risk of iatrogenic lesions, usually associated with healthcare, including dressings, vascular punctures, and prolonged decubitus21. Thus, iatrogenic injuries can often suffer complications such as contact dermatitis, ulcers, secondary skin infections, and vascular cutaneous disorders22, which could be a possible reason for the preponderance of “cellulitis and acute lymphangitis,” (L03) “cutaneous abscess, furuncle, and carbuncle,” (L02) and “purpura” (D69), as the main dermatological diagnoses registered by pediatric assistant teams.
Dermatology consultations: diagnosis and recommendations
In view of the variety of skin disorders, dermatology can perform a supporting role to pediatric hospitalists, contributing to avoiding inconsistent diagnosis and incorrect treatments, which would lead to iatrogenic complications and/or drug reactions, mainly in the pediatric population2. Thus, the exchange of knowledge and practices among dermatologists and pediatricians can confer a qualification for the assistance of complex skin conditions23.
Moreover, dermatologists can also contribute by performing complementary exams, such as skin biopsy and direct mycological examination1,9. Considering this assumption, we noted the main complementary exams in hospital consultations: laboratory tests (29.3%) and skin biopsies (10.8%), the latter performed by the dermatology team. Skin biopsies were reduced in relation to previous studies—in India10 (17.5%) and the United States23 (35%)—which may be related to different epidemiological profiles of these settings, then necessitating further investigation.
Concerning dermatology recommendations, topical presentations were the main form of medication, in concordance with the literature2,9. Diverging from research in Turkish hospital2, which pointed out moisturizers and antihistamines as major prescribing medications, our findings demonstrated topical corticoids and systemic antibiotics.
Although this study did not conduct a comparative analysis between non-dermatologists and dermatologists’ managements, Daye M et al.2 highlighted a tendency for assistant teams to prescribe treatments before dermatology evaluation in about a third of consultations, then to establish inadequate treatments in half of those hospitalizations.
About two-thirds of dermatology consultations recommended an outpatient follow-up, a higher propensity than reported by Moon AT et al.24 (48.1%) and Srinivas SM et al.10 (35.8%). Notwithstanding, disease severity and patients’ vulnerability greatly contribute to follow-up recommendations; thus, further studies are demanded to identify relations between epidemiological profiles and follow-up among different scenarios.
Pediatric dermatology and pediatrics: dialogue and contributions
Considering pediatric hospital dermatoses, both in dermatology consultations and in general pediatric wards, we noted that pediatricians demonstrated a tendency to diagnose more common and less complex cutaneous conditions, whereas dermatologists usually established more specific and defiant diagnoses, including atopic dermatitis, acne, psoriasis, and drug eruptions.
Nonetheless, our findings revealed severe cutaneous infectious—relatively common in pediatric populations—also emerged in dermatology consultations, such as scabies, impetigo, herpes virus infections, and molluscum contagiosum. This trend suggests a prominent need for training pediatricians on the diagnosis and management of dermatological disorders9. Furthermore, Dermatology consultations also represent a valuable teaching-learning opportunity, favoring the exchange of experiences and improvement of clinical practices17.
From this perspective, Daye M et al.2 and Garg T et al.4 recommended integration strategies among pediatrics and dermatology in the shape of seminars, courses, and clinical case discussions. Thus, by proposing and developing these educational activities, a field of shared knowledge can be fashioned: hospital pediatric dermatology17.
Conclusion
From this study, we outlined the profiles of dermatoses and dermatology consultations in a pediatric hospital, evidencing the prominence of inflammatory and infectious cutaneous conditions in children and adolescent populations. Moreover, vulnerabilities and shortcomings of the dermatology consultations process were also found, indicating the need for evaluations and enhancements, mainly regarding clinical data of referrals.
The acute character of various dermatoses, although not severe in many cases, reinforces the importance of both proper clinical management of cutaneous conditions, as well as the establishment of adequate criteria for dermatology consultation referrals and hospital admissions for those skin disorders.
About study limitations, we state the retrospective character of this research, based on the analysis of referrals’ registration and medical records, which may eventually present inaccuracies and/or absence of data. In addition, since dermatological diagnoses were established by dermatology teams, they can reveal a certain degree of subjectivity, strongly influenced by dermatologists’ skills.
In view of the findings and considerations presented through this study, the relevance of dermatology for hospital assistance became evident, which can provide valuable contributions to other medical specialties, including pediatrics.














