Introduction
Granular cell tumors (GCT) are rare soft tissue neoplasms with an incidence estimated in 1:1,000,000 population/year1,2. GCT has been reported in patients from all age groups but most commonly appears in the fourth and sixth decades of life3,4. Male to female ratio is variable, with some series reporting it more frequently in males while others suggest that it’s more common in females3. GCT usually appear as solitary lesions, although occasionally, they are multiple and syndromic cases have been reported5.
Most tumors arise in the oral mucosa and skin, but cases in other organs have been described1,3,4. Up to 50% of cases occur in the head and neck region, with lesions arising in the tongue representing one-third of these tumors4,6. Classically it is a slow-growing lesion with indefinite borders and a round shape, 5-20 mm in diameter, a whitish color, and a smooth surface, though ulceration may occur in a few cases4,5. While local pain is not commonly reported, some discomfort happens during tooth brushing, eating, or oral trauma7. The malignant variant is very uncommon, and only 2% of cases have been known to metastasize to distant sites4,6,8.
Case synopsis
A 10-year-old boy, otherwise healthy, presented to our department due to a hard painless nodule on the tongue. It started as a small swelling that gradually increased in size over the past 6 months.
Physical examination revealed a single whitish nodule, firm, slightly tender on palpation, and about 2 cm in size in the postero-lateral right margin of the tongue (Figure 1).
As the etiology of the lesion was unknown, and it was a relatively large lesion in a child, an incisional biopsy was done. The histology disclosed a mucosa covered by stratified squamous epithelium exhibiting reactive hyperplasia and a poorly circumscribed and infiltrative lesion on the subepithelial tissue composed of polygonal cells with small nuclei and abundant pale eosinophilic granular cytoplasm (Figure 2A to C). The cell borders were indistinct, giving rise to a syncytial appearance. The mitotic index was low, and there was a strong and diffuse expression of S100, highlighting its putative Schwannian origin. Therefore a diagnosis of granular cell tumor was established. The patient underwent a right partial glossectomy, and the surgical margins were tumor free.
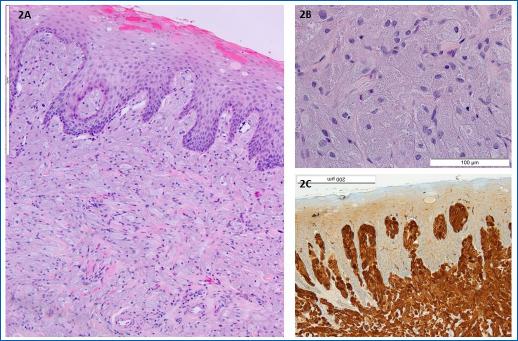
Figures 2A to C (A) H&E 100×: mucosa covered by stratified squamous epithelium exhibiting reactive hyperplasia and a poorly circumscribed and infiltrative lesion on the subepithelial tissue, (B) H&E 400×: it is composed of polygonal cells with small nuclei and abundant pale eosinophilic granular cytoplasm; pustule-ovoid bodies of Millian corresponding to larger granules surrounded by a clear halo, are also identified, (C): strong and diffuse expression of S100 in the neoplastic cells, 200×.
Discussion
Granular cell tumors (GCT) are rare soft tissue tumors, mostly benign, thought to derive from cells in the nerve sheath1,9. S100 protein is the most widely used immunohistochemical marker for these tumors, which was positive in our case1. Other immunostains positivity has also been described, such as neuron-specific enolase, cluster of differentiation 68, and calretinin4,10,11.
Histologically GCT is characterized by non-encapsulated cords, nests, or sheets of infiltrative polygonal and occasionally spindled cells with an abundant granular eosinophilic cytoplasm. Nuclei are small and centrally placed with dense chromatin4. An important histological finding reported in up to half of granular cell tumors is pseudoepitheliomatous hyperplasia of the overlying epithelium1. Therefore, if the biopsy is too superficial, GCT can be mistaken for a squamous cell carcinoma12.
As GCT generally occurs in adults in the third to sixth decades and is very rare in the first two decades of life, many other benign lesions have to be considered in the differential diagnosis, including vascular lesions, lipoma, fibroma, or mucous cyst13.
Furthermore, multiple GCTs have been rarely reported, especially in children with neurofibromatosis, Noonan’s syndrome, or growth retardation14.
Although benign GCTs have an excellent prognosis after local excision, the malignant ones have a poor prognosis, as they are not sensitive to radiotherapy or chemotherapy. Differentiation is based on histological findings, a complete history, physical examination, and other criteria, including size, rapidity of growth, invasion of nearby structures, and the presence of metastasis. Some authors consider it malignant only if it has metastasized3,8,15. Fanburg-Smith et al. have p roposed six items to consider a granular cell tumor malignant (Table 1)16. If three or more of these criteria are present, then the tumor is considered malignant, in which case it grows faster and has the potential to produce metastasis, especially to the regional lymph nodes, liver, lungs, and bone8.
Table 1 Classification of GCTs according to Fanburg-Smith et al. criteria14
| Criteria | |
|---|---|
| Increased nuclear-to-cytoplasmic ratio | |
| Pleomorphism (celular and/or nuclear) | |
| Tumor necrosis | |
| Spindling of tumor cells | |
| Vesicular nuclei with prominent nucleoli | |
| Mitotic count of > 2 in 10 high-power fields (200× field) | |
| Classification | |
| Benign | None of the criteria or focal pleomorphism |
| Atypical | 1-2 criteria |
| Malignant | ≥ 3 criteria |
Regardless of the malignancy, election therapy is the simple conservative excision of the lesion4. Relapse occurs more frequently when surgical margins are positive for tumor cells, but some studies have found local relapse even after total excision with free margin17.
This case is interesting because it is an uncommon tumor that rarely presents at such a young age. In conclusion, regardless of pediatric age, a biopsy should not be postponed whenever there is uncertainty in the clinical diagnosis.















