Introduction
Leprosy is a chronic infectious disease caused by the bacillus Mycobacterium leprae, a microorganism that has a tropism for Schwann cells of the peripheral nerves and macrophages of the skin. It has high infectivity and low pathogenicity1. Although the exact mode of transmission has not been elucidated, close contact with an infected individual in the same household or community is commonly recognized as a high-risk factor for infection2,3. Classically, a case of leprosy is diagnosed when one or more of the following findings are present-skin lesion with altered sensitivity, nerve trunk thickening, or positive skin smear4.
The operational classification created by the World Health Organization (WHO) is widely used in programs to combat leprosy around the world. This classification is based on the number of skin lesions-individuals with one to five skin lesions are classified as paucibacillary (PB), while those with six or more are classified as MB5.
Multidrug therapy (MDT) is a combination of drugs that is very safe and effective in treating leprosy and preventing the emergence of drug resistance5. Currently, the WHO guidelines recommend a three-drug regimen of rifampicin, dapsone, and clofazimine for all leprosy patients, with a duration of treatment of 6 months for PB leprosy and 12 months for MB leprosy6. Around the world, MDT is available free of charge to patients who need it upon recommendation of the prescribing physician5.
Delayed diagnosis and treatment can lead to nerve damage, loss of muscle function, paralysis, or even permanent disability7. It leads to social, economic, and psychological impacts1,2. Therefore, leprosy is still considered a major public health problem in developing countries such as Brasil, India, Myanmar, and Madagascar, even with the great worldwide progress after the introduction of MDT in the 1980s1,2.
The analysis of epidemiological data is important for the implementation of public health policies that allow for breaking the cycle of leprosy transmission, facilitating early diagnosis, and avoiding disabilities.
Objectives
To analyze leprosy indicators in Brasil between 2012 and 2021, considering the number of diagnoses, age range, namely gender, clinical form of the disease, degree of physical impairment, and therapeutic methods.
Materials and methods
This is an observational, cross-sectional, and descriptive epidemiological study. The data were obtained from SINAN, the official information system for leprosy in Brasil, available at the Information Technology Department of the Unified Health System.
Leprosy is part of the National List of Compulsory Notification of Diseases and Public Health Events. Therefore, it is mandatory for health professionals to report cases of the disease on SINAN. These data are collected by professionals from health units by filling in the notification/investigation form and the follow-up bulletin4.
This study was conducted exclusively with publicly available secondary data without the identification of subjects that followed ethical principles of resolution 196/96 of the National Health Council, which justified the lack of approval from the Ethical and Research Committee.
Results
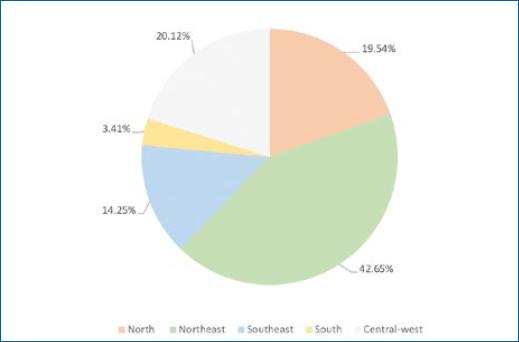
During the period between 2012 and 2021, 338,904 cases of leprosy were reported in Brasil. Most cases lived in the Northeast region (42.65%), followed by the Central-West region (20.12%), the North region (19.54%), the Southeast region (14.25%), and the South region (3.41%), respectively (Fig. 1). The Brasilian state with the highest number of cases was Maranhão, responsible for 28.10% of the cases in the Northeast region and 11.99% of the cases in the country (Fig. 2).
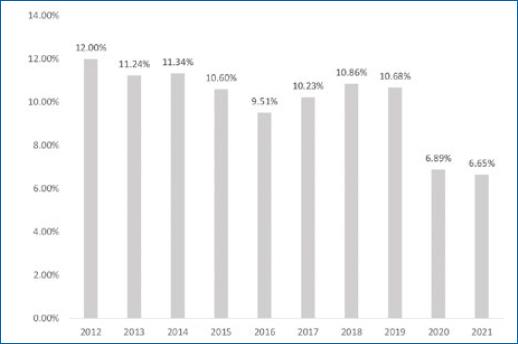
The year with the highest number of reported cases was 2012 (12%), followed by 2014 (11.34%) and 2013 (11.24%). The last year analyzed, 2021, was the one with the lowest number of cases so far (6.65%), followed by 2020 (6.89%) (Fig. 3).
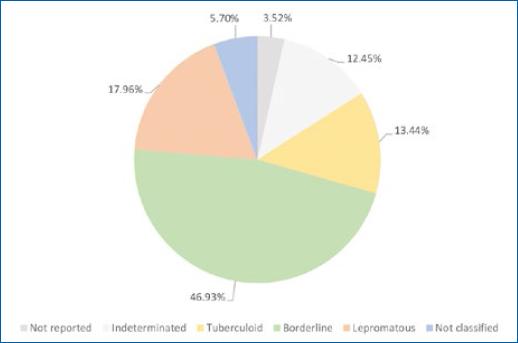
Based on the WHO classification, 25.09% were classified as PB, 74.75% as MB, and 0.15% were not reported under any of these classes of leprosy. According to the Madrid classification, most cases were considered borderline leprosy (46.93%), 17.96% as lepromatous leprosy, 13.44% as tuberculoid leprosy, 12.45% as indeterminate leprosy, 5.7% were not classified, and in 3.52% the classification was not reported (Fig. 4).
Regarding gender, leprosy was observed more in men (56.93%) than in women (43.06%). In 0.01% of the cases, gender was not reported. Most patients (50.89%) had mixed ethnicities; 24.31% were Caucasian, 12.58% were Black, 0.94% were Asian, and 0.43% were Indian. Ethnicity was not reported in 3.86% of the compulsory notification forms.
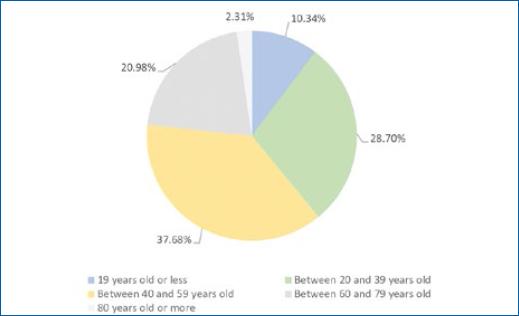
Most patients had between 40 and 59 years (37.68%), followed by the age periods between 20 and 39 years (28.7%), 60 and 79 years (20.98%), 0 and 19 years old (10.34%), and those aged 80 years or older (2.31%) (Fig.5). Around 5.91% were between 0 and 14 years.
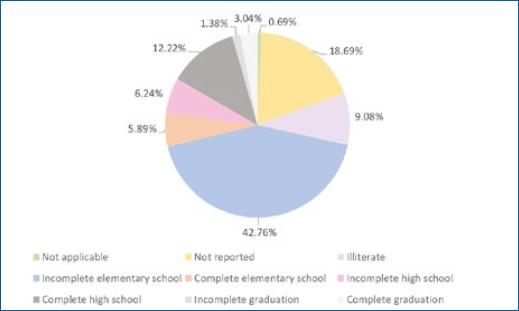
Most patients had incomplete elementary school (42.76%), 7.44% had completed elementary school, 6.24% had incomplete high school, 12.22% had completed high school, 1.38% had incomplete graduation, and 3.04% had completed graduation. A total of 9.08% of patients were illiterate (Fig. 6).
Regarding the MDT regimen, 73.32% of the patients were treated with 12 doses, 24.81% with six doses, and 1.57% were treated with alternative treatment regimens. This field was not completed in 0.3% of the compulsory notification forms.
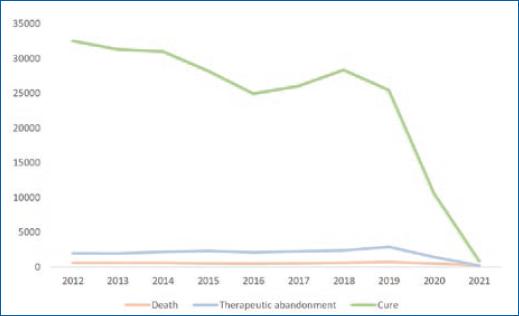
In most cases, patients were considered healed and discharged for cure (70.65%). 5.83% abandoned the treatment; however, the number of these cases reduced progressively over the years, with 2021 having the lowest number of cases abandoning treatment (1.09%). Around 1.61% of cases died of leprosy, but 2021 was also the year with the lowest number of deaths (3.91%) (Fig. 7). A total of 1.51% of patients initially reported as having leprosy were later reclassified into other diseases.
In new cases, that is, patients with characteristic signs and symptoms but who have never received specific treatment7, predominated (81.02%) over recurrences (4.48%).
No leprosy reactions were documented in 60.66% of the cases, 9.71% evolved only with type 1 leprosy reaction, 3% evolved only with type 2 leprosy reaction, and 1.37% evolved with both types of leprosy reaction. This item was not completed in 25.27% of the notification forms.
Disability was graded as 0 (absence of neural involvement), grade 1 (decrease or loss of sensation in the eyes, hands, and feet), and grade 2 (serious injuries to the eyes, hands, and feet)7,8, observed at the time of diagnosis, respectively in 54.78, 24.52, and 8.45%. Disabilities were not evaluated or not specified in the notification forms, respectively, in 4.46 and 7.76% of the cases.
Discussion
Leprosy is considered a neglected tropical disease. In the 1980s, after the introduction of MDT, there was a significant reduction in the number of cases5. However, Brasil has not yet managed to reach the level of elimination of disease, that is, a prevalence of less than one case per 10,000 inhabitants4.
Actions to reduce the burden of leprosy in the country continue to be influenced by the COVID-19 pandemic, with an impact on the diagnosis and monitoring of cases of the disease in Brasil. Although there has been a decrease in leprosy cases over the years, the sharpest reduction in the last 2 years may be related to the lower detection of cases caused by the COVID-19 pandemic4, justified by the closure of health services intended for the diagnosis of Hansen's disease, as shown in Figure 3.
In the Brasilian scenario, the inequality observed in leprosy control is notorious. The Northeast region had more than twice as many cases compared to other regions. This may be associated with the fact that this region is considered the poorest in the country, with many inhabitants living in an unfavorable socioeconomic situation. The south and southeast regions showed a reduction in cases of leprosy. The large Brasilian territorial extension and socioeconomic inequalities are cited as the main reason for this discrepancy8-10. Maranhão was the state with the highest number of cases. The endemicity of leprosy in this state is related to low values in the Human Development Index, which challenges the control of the disease9.
The predominant type observed was MB disease, which is associated with late detection of the disease, contributes to maintaining transmissibility, and worsens neurological damage8.
Regarding gender, the fact that men seek health services less and that they are more prone to Mycobacterium leprae infection in their professional environment are factors for the greater number of cases in males8.
The educational level of most patients with leprosy was very low. The lower the level of education, the greater the probability of occurrence and reactivation of leprosy, as this class has a low level of knowledge and often less understanding of treatment guidelines, preventive measures, and forms of self-care9,11. This educational deficit can also delay the diagnosis and perception of the emergence of complications of the disease11. Social conditions and educational vulnerability are associated with precarious situations of hygiene, poverty, and low socioeconomic status9.
Leprosy has a long incubation period, which is associated with the delay in diagnosis and initiation of treatment are factors for the increase in the number of cases with age progression, especially in economically active people, as shown above. The occurrence of leprosy in the age group under 15 years has a great epidemiological value, as it indicates an early exposure to the etiological agent, making it an important point for evaluating its transmissibility8.
Most cases progressed to cure. Adequate treatment is a key factor in curing the patient in order to interrupt the chain of transmissibility, thus being an important tool for controlling the disease. In addition, it plays a crucial role in preventing disabilities11.
The main social impact of leprosy occurs due to the genesis of disabilities. The complications can be responsible for permanent sequelae, resulting in social and psychological damage11. Most patients had grade 0 disability at the diagnosis moment. However, a considerable percentage of the patients were not evaluated for disabilities or not specified in notification forms.
Current leprosy control strategies rely on early diagnosis and prompt treatment to minimize the progressive morbidity of leprosy and hopefully interrupt transmission from clinically active cases3.
Conclusion
The limitation of this study was the impossibility of analyzing some information due to failures to fill in the SINAN forms.
Despite significant improvements in leprosy control in recent decades, the disease persists as a public health problem. Identifying behavioral and environmental risk factors for developing leprosy is a difficult task because of the long incubation time of the disease3. We emphasize the need to expand the field of leprosy research in order to understand its epidemiology in Brasil and have an early intervention to reduce late diagnoses and consequent physical disabilities.