Introduction
Keratosis lichenoides chronica (KLC) is an uncommon mucocutaneous disorder originally described in 1895 by Kaposi, who called it ‘lichen ruber acuminatus morbilliform’1. Later, in 1938, Nekam took note of acrosyringeal hyperkeratosis in the case published by Kaposi and named the disease ‘porokeratosis striata lichenoides’ despite the lack of coronoid lamella2. Finally, in 1972, Margolis et al. introduced the nomenclature currently used—‘KLC’3.
Case description
A 56-year-old male, otherwise healthy, presented to the dermatology department with a 1-year history of persistent asymptomatic cutaneous lesions predominantly affecting the limbs and face. On examination, multiple keratotic violaceous papules and plaques were distributed over the dorsum of his hands and fingers (Fig. 1A), as well as on the medial aspect of both thighs, where they were arranged in a linear pattern (Fig. 1B). On his face, there were erythematous and squamous lesions located mainly in the midfacial area, resembling seborrheic dermatitis (Fig. 1C). Mucous membranes, genital region, scalp and nails were spared. The remaining physical examination was unremarkable and his routine blood tests, including viral serologies and autoimmunity markers, were normal.

Figure 1 Clinical features. A: keratotic papules on the thighs, some arranged in a linear pattern; B: keratotic violaceous papules over the dorsum of the hand; C: facial seborrheic dermatitis-like eruption.
There was no familiar history of similar complaints.
A skin biopsy performed on a thigh lesion revealed irregular acanthosis and hyperkeratosis with alternating areas of orthokeratosis and parakeratosis. In the upper dermis, there was a dense lichenoid infiltrate composed of lymphocytes and plasma cells, associated with multiple foci of vacuolar degeneration of the basal epidermal layer and apoptotic keratinocytes (Fig. 2).
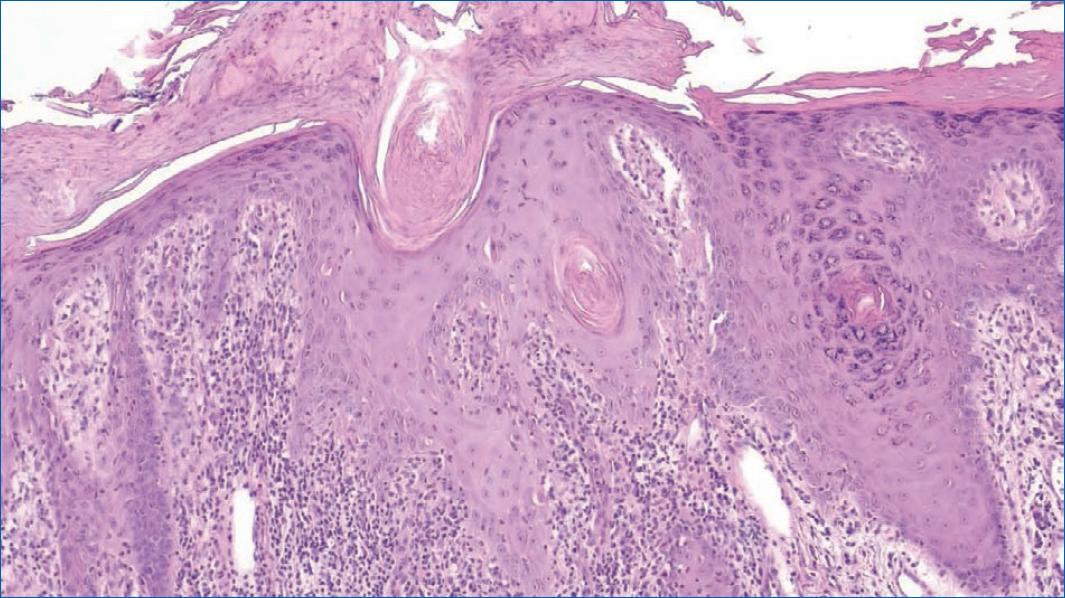
Figure 2 Histopathological aspects: irregular acanthosis with focal parakeratosis, apoptotic keratinocytes at various levels of the epidermis and mixed lichenoid infiltrate in the superficial dermis (H&E, 10x).
This combination of clinical and histological findings strongly suggested the diagnosis of KLC. The patient declined to be tested for the nucleotide-binding domain and leucine-rich repeat-containing protein 1 (NLRP1) gene. Treatment was initiated with acitretin 35 mg daily, in addition to the topical application of tacrolimus 1% ointment on the face and clobetasol propionate ointment 0.05% on the extremities. At 6 months follow-up, the lesions on his hands had significantly improved. However, other lesions showed milder responses to the treatment.
Discussion
Keratosis lichenoides chronica (KLC), also known as Nekam's disease, is a rare dermatosis of uncertain etiology. It appears most frequently in adults, with a peak of incidence in the 4th decade and slight predominance in males1,2,4.
Previously perceived as the expression of other inflammatory conditions such as lichen planus, lupus erythematosus or lichen simplex chronicus5,6, KLC is now considered a distinct entity since the detection of a gain-of-function mutation in the nucleotide-binding domain and leucine-rich repeat-containing proteins 1 (NLRP1) gene in a family with semi-dominantly inherited KLC7.
NLRP1 is an inflammasome sensor protein in high levels in keratinocytes and cutaneous fibroblasts. It is thought that the gain-of-function mutation in the NLRP1 gene causes constitutive inflammasome activation and leads to reactive keratinocyte proliferation7,8. However, further studies are required to fully comprehend the pathogenesis of both familiar and sporadic cases.
Clinically, KLC is characterised by lichenoid or keratotic violaceus papules arranged in a linear or reticulated pattern, especially on the limbs4. A seborrheic-like dermatitis eruption on the face is also a common finding of this disorder4. Less frequent features include oral and genital ulcerative lesions, palmoplantar keratoderma and onychodystrophy which are found, respectively, in 50, 40 and 30% of cases1,9,10.
Regarding histology, typical findings are hyperkeratosis with focal parakeratosis, irregular acanthosis alternating with areas of atrophy, vacuolar degeneration of keratinocytes at dermoepidermal junction and chronic inflammatory infiltrate in the upper dermis consisting of lymphocytes, histiocytes and plasma cells (often around infundibula and acrosyringia)4,5.
Several inflammatory dermatoses, such as lichen planus, lichen planus-psoriasis overlap, lichen planopilaris, pityriasis rubra pilaris and cutaneous lupus erythematous may mimic KLC10.
Keratosis lichenoides chronica (KLC) has a chronic and progressive course and is highly resistant to therapy11,12. The most effective treatment consists of oral retinoids at a dose of 0.3-0.6 mg/kg/day2,11, although complete responses are infrequent11. Phototherapy (psoralen plus ultraviolet A and narrow-band ultraviolet B) can be helpful, especially as an adjuvant treatment4,11. Topical treatment, as well as systemic steroids, other immunosuppressants and antimalarials, are usually ineffective2,12.
This case serves to highlight KLC as a well-defined disease with consistent clinical and histological characteristics. Its pathogenesis is still not fully understood, although recent progress has been made with the discovery of the possible contribution of the NLRP1 gene.
Despite its rarity, KLC is an entity that dermatologists should keep in mind, with the aim of detecting more cases and performing more investigations on both pathophysiology and therapeutical approaches.














