Introduction
Mantle cell lymphoma (MCL) is a B-cell NHL that develops from malignant B-lymphocytes within a region of the lymph node known as the mantle zone. MCL represents only 6% of all NHL1.
Many affected individuals have widespread disease at diagnosis, with involved regions often including multiple lymph nodes, the spleen, and, potentially, the bone marrow, the liver and the gastrointestinal tract. Skin involvement is rare and is associated with progressive disease1.
Our case report describes one of the rare cases of cutaneous involvement by an MCL.
Clinical significance
We describe the case of a 73-year-old female patient with priors of an MCL and a total left knee replacement 1 year ago.
Around 9 months ago, the patient started experiencing asthenia and undesired weight loss. Blood work showed anaemia and neutropenia, and clinical examination detected cervical lymphadenopathies. Biopsy of a lymph node diagnosed an MCL. Bone marrow biopsy showed involvement of the bone marrow and a positron emission tomography/computed tomography scan revealed multiple lymphadenopathies, thus an MCL stage IVB.
The patient underwent six cycles of chemotherapy with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone, with disease control, followed by maintenance rituximab therapy, currently on the second cycle.
The patient presented to the dermatology department with patches on the left leg, with 3 months of evolution.
On examination, the patient presented with infiltrated, confluent, shiny erythematous to violaceous patches and plaques on the anterior surface of the left knee and leg and on the arthroplasty scar (Fig. 1), with no associated complaints and no other relevant cutaneous lesions.

Figure 1 Erythematous-violaceous patches and plaques on the anterior surface of the left knee and leg.
Blood work showed aggravation of anaemia, neutropenia and an elevation of LDH de novo.
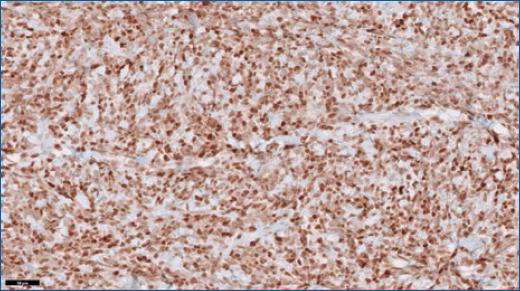
A skin biopsy revealed dense occupation of the skin by a diffuse patterned lymphoid proliferation, with intermediate-sized cells, scarce cytoplasm, hyperchromatic nuclei and irregular borders (Figs. 2 and 3). In immunohistochemistry, the cells were positive for CD20, CD5, cyclin D1 and Bcl-2, and negative for CD3 and CD10 (Figs. 4 and 5). These findings are compatible with cutaneous involvement by MCL.
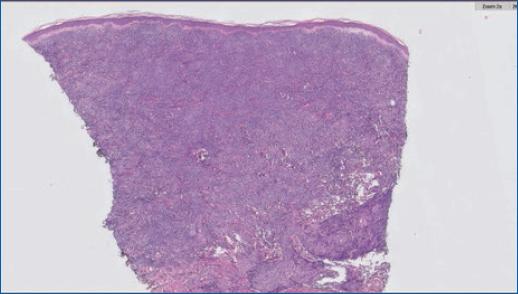
Figure 2 Skin biopsy with the dense occupation of the skin by a diffuse patterned lymphoid proliferation, sparing only a straight subepidermal band (grenz zone).]
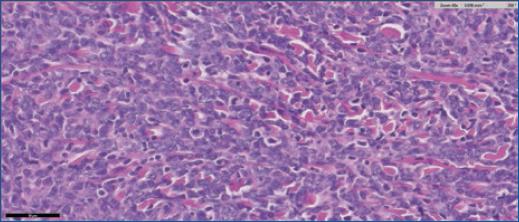
Figure 3 Lymphocytes with intermediate-sized cells, with scarce cytoplasm, hyperchromatic nuclei, and slightly irregular nuclear borders. Some mitotic figures can be seen.
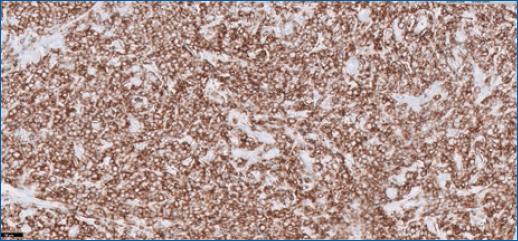
Figure 4 In immunohistochemistry, the cells were positive for CD20, therefore, from the B-lymphocyte lineage.
Maintenance therapy was stopped and the patient underwent radiotherapy on the left leg with regression of the lesions. The patient is currently under chemotherapy with R-BAC (rituximab, bendamustine, and cytarabine).
Discussion
Mantle cell lymphoma (MCL) is an uncommon form of NHL, accounting for 5–7% of all cases of NHL. It develops from malignant B-lymphocytes within a region of the lymph node known as the mantle zone1. Around 90% of patients with MCL have a mutation that leads to the overproduction of a protein called cyclin D1 in the lymphoma cells2.
It affects mostly men who are usually 60–70 years old1.
The disease is typically widespread at diagnosis. Extranodal involvement, especially of the gastrointestinal tract, spleen and bone marrow, is fairly common in MCL3.
In the classification of World Health Organization, MCL is listed as an extracutaneous lymphoma secondarily involving the skin2. Primary involvement of the skin with MCL is controversial and extremely rare. Secondary involvement is described to occur in 2% of all MCL cases and in 17% of cases with stage IV MCL, with about 30 cases reported4-6. This case was also a stage IV MCL.
Most cases report skin involvement of the trunk, followed by the face, upper limbs and less commonly, the lower limbs and abdomen. Also, the primary lesions are usually described as erythematous nodules but can also be papules and plaques2,4-6. In this case, the patient presented with patches and plaques in only one lower limb at the site of a previous orthopaedic surgery which has never been described to our knowledge.
The immunohistochemical profile of the MCL of our patient was comparable to that of published cases. According to the guidelines, the diagnosis of MCL should be established on the basis of morphological examination and immunophenotyping with the detection of cyclin D1 protein overexpression. Histologically MCL is composed of diffuse or nodular proliferations of B lymphocytes positive for B-cell markers, like CD79a, CD19, CD20, CD22 and CD5 and usually negative for CD10, CD23 and bcl-66. In this case, the skin biopsy revealed a diffuse lymphoid proliferation with tumour cells positive for B-cell markers—CD20 and CD5, negative for CD3 and CD10 and overexpression of cyclin D1.
Patients who develop the cutaneous disease with widespread MCL typically have a progressive disease and, therefore, poor prognosis4.
Although rare, skin involvement can be the first complaint of MCL in some cases and therefore, its first manifestation. Since this type of lymphoma is associated with a poor prognosis, a quick diagnosis and rapid treatment are crucial for survival.