Introduction
Breast cancer is the most frequently diagnosed cancer in women and ranks second among causes of cancer-related death. Cancer patients may experience several dermatological manifestations during treatment, including cutaneous adverse effects of chemotherapy1,2. Moreover, in immunosuppressed patients, the most common infections are often associated with atypical clinical presentations.
Herein, we describe a case of synchronous presentation of HFMD and PPE in a breast cancer patient undergoing chemotherapy treatment.
Case presentation
A 36-year-old female patient presented to our outpatient dermatology department with a 1-week history of palmoplantar numbness and tingling associated with painful lesions on the palms and soles. She denied accompanying systemic symptoms. Her 18-month-old daughter had been diagnosed with HFMD 3 days before the beginning of cutaneous manifestations. Her medical history included breast cancer cT2N2M0. She was going through the third cycle of neoadjuvant chemotherapy with doxorubicin and cyclophosphamide. Examination revealed multiple erythematous purpuric papules, patches, vesicles and bullae on the palms and soles (Fig. 1). There were no mucosal lesions.

Figures 1A and B Clinical picture-hand, foot and mouth disease & palmo-plantar erythrodysesthesia. A: erythematous purpuric papules and patches on the palms, B: erythematopurpuric papules, patches, vesicles and bullae on the soles.
Two skin biopsies were performed, one on a palmar vesicle and the other on an erythematous papule on the arm. After a discussion with the oncology department, it was decided to delay the next chemotherapy cycle. Treatment consisted of betamethasone 1 mg/gm cream twice daily. After 1 week, there was a dissemination of the dermatosis associated with the recent onset of fever and dry cough. Laboratory studies revealed leucopenia 1.10 × 109 L (normal range (NR) 4-11 × 109/L), neutropenia 0.24 × 109/L (NR 1.9-7.5 × 109/L) and high C-reactive protein 12.2 mg/dL (NR < 0.5 mg/dL). There was a positive IgM and IgG serology for coxsackievirus.
The vesicle biopsy showed intraepidermal spongiosis, vesicle formation, epidermal necrosis and mixed inflammatory infiltrate, with eosinophils and lymphocytes, in the superficial dermis. These findings were consistent with HFMD (Fig. 2). Histopathological examination of the erythematous papule on the arm revealed orthokeratotic hyperkeratosis, atypical basal keratinocytes, oedema of the superficial dermis with a perivascular lymphocytic infiltrate and erythrocyte extravasation. These findings were compatible with PPE (Fig. 3).
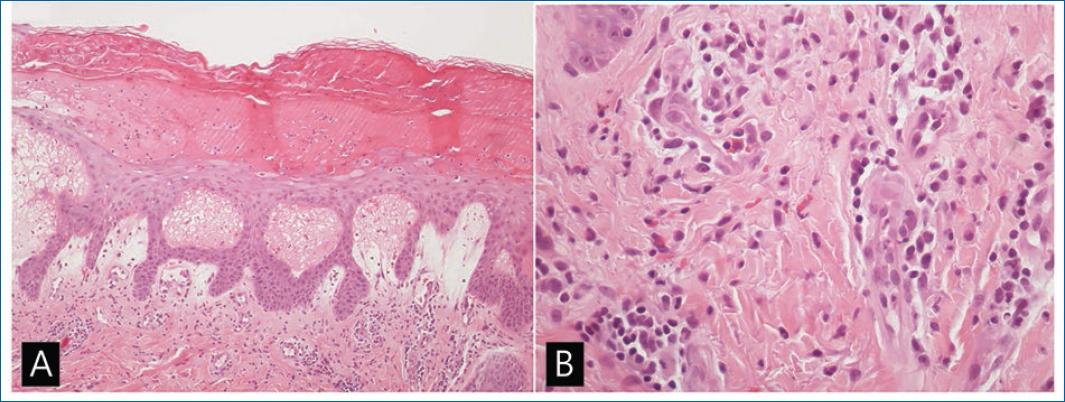
Figures 2A and B Hand, foot and mouth disease-skin biopsy. A: intraepidermal spongiosis, ballooning and reticular degeneration with intraepidermal vesicle formation and epidermal necrosis (H&E stain, magnification ×40), B: inflammatory infiltrate with lymphocytes, eosinophils and neutrophils in the superficial dermis. Vascular dilatation and erythrocyte extravasation (H&E stain, magnification ×100).
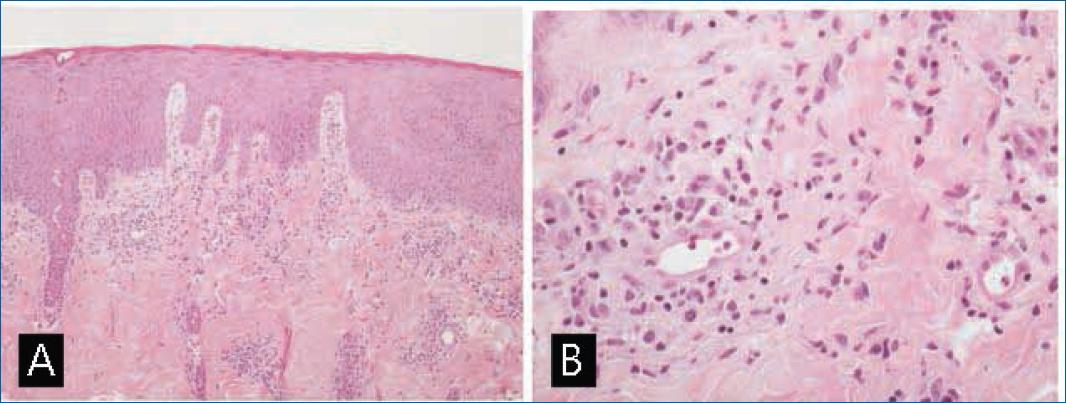
Figures 3A and B Palmo-plantar erythrodysesthesia—skin biopsy. A: irregular acanthosis, orthokeratotic hyperkeratosis and dermal oedema (H&E stain, magnification ×40), B: perivascular lymphocytic infiltrate and erythrocyte extravasation (H&E stain, magnification ×100).
Two weeks later, the dermatosis regressed, and blood work was normal. The patient went to the oncology consultation to schedule the next chemotherapy cycle. There was a clinical recurrence of mild PPE without the need to discontinue chemotherapy.
Discussion
Considering the clinical and epidemiological features described, the main differential diagnoses considered were HFMD, PPE, erythema multiforme (EM) and exanthem induced by other viruses. HFMD and PPE are mimickers of each other, and their diagnosis in this patient was only possible through histopathology.
Hand, foot and mouth disease (HFMD) affects approximately 11% of exposed adults, but fewer than 1% of infected adults develop clinical manifestations3. Clinically, HFMD is characterized by fever, acral vesicular exanthema and painful stomatitis4. In our case, epidemiologic and clinical features led to the suspicion of HFMD. Progression with disseminated dermatosis was a concern in our patient due to her immunocompromised condition.
There is relatively limited histopathologic reporting on HFMD5. This likely reflects that HFMD in children is usually recognized by clinicians and does not typically require histopathology for diagnosis. In most cases reported in the literature, histopathological findings include spongiosis, extravasation of red blood cells and leukocytoclastic6,7. In our case, a skin biopsy taken on a vesicle of the hand revealed features consistent with a viral infection, namely HFMD. Our case's main clinical differential diagnosis included EM and other viral infections. However, the absence of vacuolar alteration at the dermoepidermal junction and the presence of eosinophils in the inflammatory infiltrate make the EM hypothesis unlikely. On the contrary, the lack of classic viral cytopathic changes excludes a herpesvirus infection.
Palmoplantar erythrodysesthesia (PPE) is a toxic dermatologic reaction associated with specific chemotherapeutic agents, such as pegylated liposomal doxorubicin6,8,9. We were concerned about the need for chemotherapeutic dose reductions or a switch to other drugs. The decision to delay the next chemotherapy cycle and the topical treatment ameliorated symptoms and helped to prevent the progression of both PPE and viral infection. Synchronous presentation of HFMD might have contributed to the worsening and possibly to overrating the PPE. The recurrence of mild PPE after resuming chemotherapy supports this observation. The histopathologic features in PPE most commonly described are dyskeratotic keratinocytes, basal layer vacuolar degeneration, mild perivascular lymphocyte infiltrate, spongiosis, hyperkeratosis, and parakeratosis6. Our palmar papule biopsy revealed findings consistent with PPE.
To the best of our knowledge, the synchronous presentation of HFMD and PPE has not yet been reported in the literature. In our case, concomitant PPE and immunosuppression might have been responsible for the atypical presentation, longer course and clinical severity of HFMD.














