Introduction
Sporotrichosis is a chronic subcutaneous or lymphocutaneous granulomatous infection1, caused by thermodimorphic fungi of the genus Sporothrix2. The disease has a worldwide distribution, especially in tropical and subtropical areas, as temperature and humidity favor the spread of the fungus3. Its predominance in populations with a lower socioeconomic profile makes this pathology a candidate for inclusion in the World Health Organization list of Neglected Tropical Diseases4 as a public health problem of extreme importance.
Sporotrichosis is the most prevalent subcutaneous mycosis in Latin America, still considered endemic in countries such as Brazil, Colombia, Venezuela, and Argentina5. Several Brazilian states have a particularly high incidence and compulsory notification of the disease, such as São Paulo, Pernambuco, and mainly, Rio de Janeiro6, which was considered a hyperendemic region since 1998, and has been responsible for 32% of hospitalizations and 23% of deaths in recent decades7.
There are two main routes of transmission of the disease to humans, after traumatic inoculation of the spores or mycelial fragments of the fungus into the dermis4, either by direct contact with decomposing organic matter or infected soil, or by animal scratches, in which felines, especially cats are particularly important5. Since the 1990s, the latter route has shown a greater correlation with the increase in the number of severe cases in Brazil2.
It is extremely important, therefore, to consider the epidemiological data, clinical characteristics, and outcome of patients with sporotrichosis, with the aim of reducing the number of cases, creating effective measures to promote health and prevent the disease, in addition to more appropriate and early therapy.
Methodology
This is a descriptive, observational, and single-center case series study, carried out at the dermatology service of the Center for Biological and Health Sciences at the University of the state of Pará, in Belém, Pará, one of the reference centers in secondary care for general and tropical dermatological diseases in the region. The research was carried out after approval by the University’s Research Ethics Committee, opinion nº 5.647.696, and authorization from the coordination of the University’s Dermatology Service.
This is a convenience sample and consists of patients with sporotrichosis treated in the years 2020-2022, with a positive epidemiological history (contact with a cat) and confirmed by anatomopathological examination and culture for fungi.
A standardized protocol authored by the researchers was used to collect data from the medical records. The variables collected were epidemiological data, clinical aspects of the lesions, type of treatment, and clinical outcome.
Results
Seven patients diagnosed with sporotrichosis were analyzed, five females and two males, with ages ranging from 10 to 53 years (mean 32 years) (Table 1). Four had no previous comorbidities, one had systemic arterial hypertension and type 2 diabetes mellitus (Case 1), one had severe mental retardation (Case 6), and one suffered from antiphospholipid syndrome (Case 7 - Fig. 1). Only one patient had contamination by fomites, while the others had direct inoculation through contaminated cat scratches, and only one feline died within a period of 3 months.
Table 1 Epidemiological and clinical data of the 7 patients diagnosed with sporotrichosis in the period from 2020 to 2022 at the Dermatology Clinic
| No | Sex | Age | Occupation | Comorbidities | Cutaneous lesions | Localization | Treatment |
|---|---|---|---|---|---|---|---|
| 1 | M | 33 | Teacher | AH, DM2 | Ulcerated erythematous nodule (1 cm × 0.8 cm), linear infiltrated erythematous plaque (8 cm × 1.5 cm) | Left wrist Right leg | Itraconazole 200 mg/day 6 months |
| 2 | F | 53 | Home worker | - | Two erythematous nodules, one exulcerated with purulent discharge | Forearm and left first finger | Itraconazole 200 mg/day for 7 months |
| 3 | F | 26 | Occupational therapist | - | Erythematous nodule with an ulcerated center | 3rd right finger | Itraconazole 200 mg/day for 4 months |
| 4 | F | 42 | Day laborer | - | Erythematous nodule with an ulcerated center | 3rd right finger | Itraconazole 200 mg/day for 7 months |
| 5 | F | 22 | Veterinary | - | Discretely infiltrated erythematous edge ulceration with purulent background | Metacarpophalangeal area of the 1st left finger accompanied by erythematous nodules | Itraconazole 200 mg/day for 2 months Itraconazole 400 mg/day for 2 months Potassium iodide 3 mL/day for 3 months |
| 6 | M | 10 | Student | Severe mental retardation | Erythematous plaque with an ulcerated center covered by a serohematic crust with clear limits and regular contours measuring 1.0 cm × 1.5 cm | In the 1st right finger | Itraconazole 200 mg/day for 9 months |
| 7 | F | 38 | Administrator | Anti-phospholipid syndrome Under treatment with AAS 100 mg/day | Erythematous papules and nodules, some ulcerated, with regular contours and well-defined limits, ranging from 0.2 cm × 0.2 cm to 0.7 cm × 0.7 cm | In the upper limbs | Itraconazole 200 mg/day for 12 months Amphotericin B 0.15% eye drops every 3/3 h for 4 months |
DM2: diabetes mellitus type 2; AS: antiphospholipid syndrome; M: male; F: female.
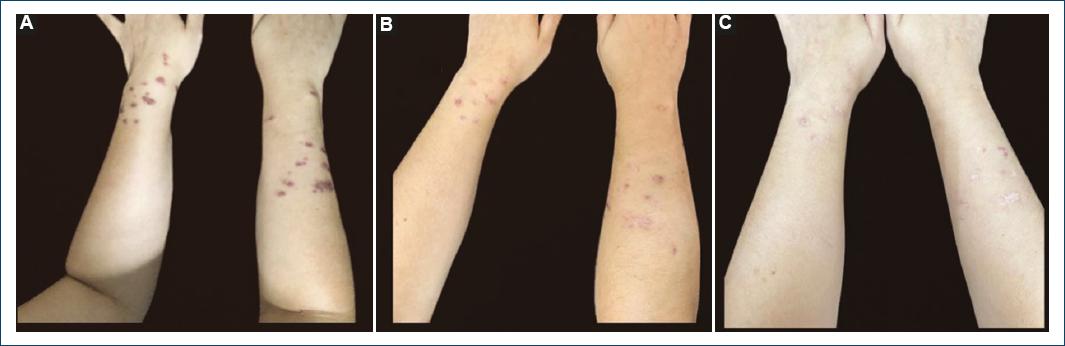
Figure 1 Cutaneous lesions in case 7. Erythematous papules and nodules, some with ulceration, with regular borders and well-defined limits, on the upper limbs, after using itraconazole for A: 2 months, B: 3 months, and C: 6 months.
All patients presented ulcerated erythematous nodules at the beginning of the condition, four with a linear arrangement of nodules in the lymphatic path (Cases 1, 2, 5, and 7 - Fig. 2), and three had palpable painful lymphadenopathy with a fibroelastic consistency (Cases 1, 3 and 7). All patients were treated with itraconazole 100 mg, 2 pills a day for 4-12 months (average 7 months), depending on treatment response and complications during treatment.
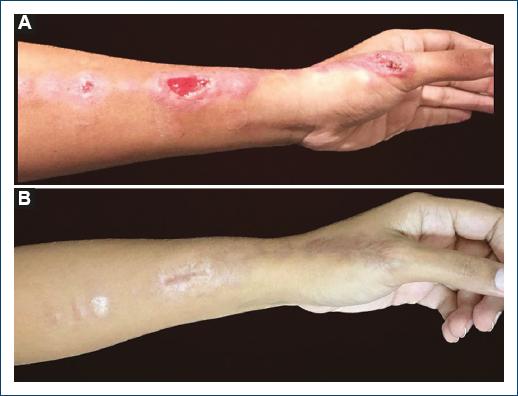
Figure 2 Cutaneous lesion in case 5. Erythematous nodules and plaques in a linear distribution with subsequent ulceration localized to the thumb and forearm. A: before starting treatment and B: 5 months after using itraconazole and potassium iodide.
Case 5 presented secondary bacterial infection in two different moments and needed additional antibiotic therapy. After this last episode, there was a progressive worsening of the sporotrichosis, requiring the association of itraconazole with potassium iodide 6 mg/day for 3 months.
Case 7, after 1 month of itraconazole 200 mg/day, complained of conjunctival hyperemia and blurred vision in the left eye, being diagnosed with ocular sporotrichosis. Amphotericin B 0.15% eye drops every 3 h for 4 months.
All 7 patients in the study progressed to cure, with complete resolution of the lesions, and all patients were still cleared after 1 year of follow-up after drug withdrawal.
Discussion
Sporotrichosis is the most common subcutaneous mycosis in the world, caused by dimorphic and geophilic fungi, of the species Sporothrix spp.1, being considered endemic in tropical, subtropical, and temperate zones with hot and humid climate3, such as the one in which the study was carried out, which favors the growth of saprophytic fungi8. Sporotrichosis, although not a pathology with high morbidity, except in the disseminated forms, is responsible for great disability, directly affecting the quality of life of affected individuals9, and is sometimes considered an occupational disease for groups of potential contamination10.
The pathogen is usually found in the soil and plants, with the agent being inoculated into the skin or mucous membrane due to trauma, which is why it has been known as “gardener’s mycosis” for a long time6. On the other hand, in Brazil, sporotrichosis is mainly due to zoonotic transmission, through the bite or scratches of felines contaminated with the fungus11, usually Sporothrix brasiliensis. It is important to emphasize that most patients in the present study were contaminated in this way, corroborating with the current literature. No age group or sex is spared from this infection, given that its occurrence depends on the fungus in the environment and the inoculation point, however, a higher frequency of occurrence in males is noted, being attributed to their greater risk of exposure to the pathogen8. This male predominance was not observed in this current study (only two male patients) probably explained by the frequent transmission by cats.
As for the pathogenesis, the cell wall of the pathogen induces an innate immune response, especially from S. brasiliensis, and the host reacts through a humoral and cell-mediated reaction, with CD4+ T cells with a mixed Th1 and Th17 immune response, capable of stimulating the secretion of cytokines such as interferon-gamma, tumor necrosis factor-alpha, and interleukin-17a, which, in turn, activate macrophages and neutrophils for fungal elimination12,13. The variability of response depends both on the factors related to the parasite itself and the immunoinflammatory capacities of the host and may explain the great clinical variability of the disease, dividing it into two large groups: cutaneous and extracutaneous, the first of which is subdivided into lymphocutaneous and fixed cutaneous14. The type of immune response is of paramount importance, as in this study, the extracutaneous form occurred in a patient with active autoimmune disease under treatment with acetylsalicylic acid 100 mg/day, which may have interfered with the immune response.
Incubation period remains uncertain, ranging from days to months, with an average of 3 weeks15. Cutaneous lesions progressively develop in the form of papules or nodules, and the site of inoculation can ulcerate, characterizing the fixed form of cutaneous sporotrichosis6. However, up to 4 weeks after the trauma, multiple painless nodules can develop along the lymphatic vessels, usually in the hands and lower limbs, characterizing lymphocutaneous sporotrichosis7, responsible for approximately 80% of cases6. Lesions can increase in size, become verrucous, nodular, or ulcerated, known as “sporotrichotic cancer”6 and in addition, lesions often extend to the lymphatics and these satellite lymph nodes can ulcerate and form fistulas as well16. More than half of the patients in this study expressed this lymphocutaneous clinical form, confirming literature findings.
Due to the diversity of clinical presentations, sporotrichosis may be clinically similar to cutaneous tuberculosis, American mucocutaneous leishmaniasis, chromoblastomycosis, paracoccidioidomycosis15, in addition to pyoderma gangrenosum and cat scratch disease6.
Disseminated or hematogenous sporotrichosis is rare and usually occurs in severely immunocompromised patients9, such as alcoholism, diabetes, acquired immunodeficiency syndrome, paraneoplastic syndromes, and use of immunosuppressive drugs15. It can affect several organs and systems, such as central nervous system, osteoarticular, ocular, and pulmonary17. Among the extracutaneous manifestations, the ocular mucosa is most commonly affected6, as the only extracutaneous form described in the study. Anatomical criteria and the source of infection explain this localization, which presents either as an adnexal infection, affecting eyelid, conjunctiva and lacrimal sac, or an intraocular infection18, with exogenous or endogenous endophthalmitis. Among ocular lesions, 82% are limited to the eyelids, mainly caused by Sporothrix schenckii, S. brasiliensis, and Sporothrix globosa19, predominantly affect children, with a history of trauma by plant material and wood20. Eyelid lesions can be primary or due to lymphocutaneous lesions from hematogenous dissemination, presenting as papules or ulcerated nodules19. There is also conjunctival sporotrichosis, with most cases reported in the current literature in Brazil, where no previous trauma was reported, although contact with cats has been reported in 90% of patients18, like the 7th case of this series. This situation can mimic several infectious or non-infectious diseases, and it is necessary to confirm the diagnosis through mycological examination20.
The gold standard for the diagnosis is based on biopsy, aspirates from abscesses, sputum, blood, synovial, and cerebrospinal fluid, based on the isolation and identification of Sporothrix species in culture and polymerase chain reaction15. Direct microscopy has low sensitivity and specificity in humans, presenting the “cigar-shaped” pattern, usually in immunosuppressed individuals21, however, this method is very sensitive in animals6. All patients had diagnostic confirmation both by biopsy with histopathological study and culture. The Splendore-Hoeppli phenomenon (sulfur granules) in the histopathological examination may suggest a diagnosis of sporotrichosis, however, it is not specific, considering that it may be present in other granulomatous diseases22. Serology is usually reserved for the diagnosis of systemic or atypical forms, in addition to helping to monitor treatment and withdrawal of medications in more complex clinical presentations12, not being used in this study for any of these purposes.
The therapeutic choice depends on the clinical form of the disease, the immune status of the host, and the species involved23. At present, in Brazil, the drugs available are itraconazole, potassium iodine (KI), terbinafine, and amphotericin B6. Itraconazole, used in all patients in this series, is considered the medication of choice due to its efficacy, dosage convenience, and can be administered continuously or in pulses24, from 100 mg to 400 mg/day, starting, preferably, with the minimum dose25. It should be emphasized that all azoles are contraindicated in pregnant women, and they inhibit cytochrome P450 and, therefore, drugs metabolized by this enzymatic system, such as warfarin, anticonvulsants, statins, and oral hypoglycemic agents are contraindicated15, due to the drug interactions. Follow-up between 1 and 2 months with laboratory tests is advised.
KI is mostly used in countries with limited resources and in immunoreactive forms such as erythema nodosum or reactive arthritis, due to its immunomodulatory effect4, which is why it was associated with itraconazole in a patient with an unsatisfactory response to monotherapy for 3 months. Terbinafine is indicated in the case of contraindication to the aforementioned drugs. As this drug is metabolized through CYP2D6, it presents fewer drug interactions26 and is, therefore, useful in elderly patients or patients with multiple comorbidities. The recommended dose is 250 mg/day, which can be doubled in adults6.
Amphotericin B is reserved for severe life-threatening cases and in pregnant women27, with efficacy between 90% and 100%26. Topical amphotericin B for 4-12 months of treatment, alone or associated with an oral antifungal, is the treatment of choice in intraocular infections but requires continuous renal evaluation due to its nephrotoxic potential18. In case 7, amphotericin eye drops were used for 4 months to treat the conjunctival presentation.
Treatment should be maintained until clinical cure, that is, when there is no disease activity, with an average duration of 4 months8. In addition to drug treatment in humans, it is necessary to treat infected cats as well as to incinerate animals killed by the disease, to prevent the spread of the pathogen in the soil6.
Conclusion
The present study provides demographic data, clinical characterization, and its diversities, in addition to the types of treatment used in medical practice in a reference center in northern Brazil, an endemic area of the disease. Data emphasize the importance of recognizing the clinical forms to enable early diagnosis and adequate treatment of sporotrichosis, as well as the notification of the disease to obtain a more reliable epidemiology, to reduce the number of disease cases and their morbidity.














