Introduction
Herpes simplex virus (HSV) infection is the leading cause of genital ulcers worldwide. HSV type 2 (HSV-2) is the most frequently associated serotype; however, genital lesions can also be caused by HSV type 1 (HSV-1), presenting with a less severe form and with less chance of recurrence1-4. The incubation period of the virus can range from 2 to 12 days, with an average of 4 days1. Primo-infection is usually asymptomatic, with symptomatic patients showing multiple, widespread, and painful ulcerations on the genitalia2.
In recurrences, the most common presentation is characterized by 2-3 mm erythematous papules, followed by formation of clustered vesicles with citrine content that break up and give rise to painful ulcerations1,4,5. However, in immunosuppressed patients, HSV infection may present in different forms such as generalized papular eruption, verrucous papules mimicking condyloma, and more rarely as a pseudotumoral hypertrophic form, which can simulate squamous cell carcinoma5-8.
These atypical presentations of HSV infection require a high degree of clinical suspicion, as well as knowledge of specific therapeutic modalities.
In this context, the authors report a case of hypertrophic genital herpes (HGH) in a patient with concomitant infection by human immunodeficiency virus (HIV), which was unsuccessfully treated with oral antivirals, and resolve after surgical excision.
Case report
A 55-year-old female patient was referred to the Pathology of the lower genital tract Clinic of the Santa Casa de São Paulo Hospital (Brazil), by the primary health care unit. She reported a painful vulvar vegetating mass, with approximately 1 year of evolution and progressive growth. The patient was diagnosed with HIV infection 22 years ago, with good adherence to the antiretroviral therapy, and an undetectable viral load (3 months before). She denied other comorbidities or chronic medication and reported that she was not sexually active for the past 20 years.
A lesional biopsy performed in primary healthcare suggested a herpes virus infection. Thus, the was treated with oral acyclovir at the maximum dose (800 mg 4/4 h) for about 3 months with continuous-lesional growth.
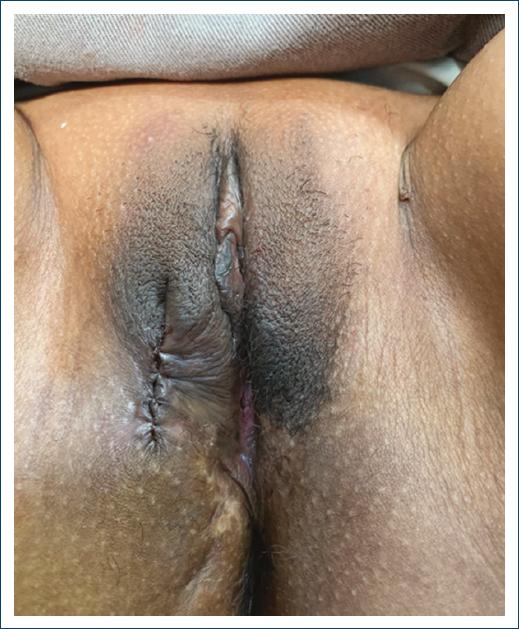
General physical examination was normal and vulvar examination revealed a rounded exophytic mass, with granulomatous appearance, ulcerated areas, and covered with purulent secretion, with approximately 4 cm, in the lateral face of the right labia majora (Fig. 1). In this context, the hypothesis of HGH was considered. Moreover, due to the failure of acyclovir therapy, the patient underwent surgical excision under local anesthesia (Fig. 2). Topical imiquimod was not part of the treatment of the patient reported in this case. The medication was unavailable in the service.

Figure 1 Pseudotumoral hypertrophic genital herpes simplex virus infection in the right labia majora.
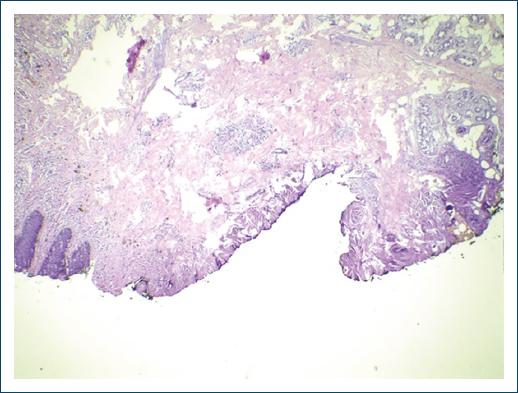
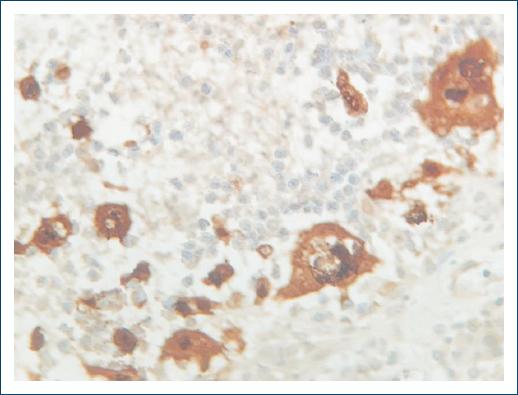
The final histopathological analysis revealed an ulcerated herpetic vulvitis with an intense acute inflammatory reaction and multinucleated cells (Fig. 3). Immunohistochemistry revealed immunoexpression of associated HSV-1 and HSV-2 (Fig. 4). Therefore, it was decided to maintain oral acyclovir (800 mg 4/4 h) for 30 days. After a follow-up of 12 months, the patient remains stable with no recurrences.
Discussion
HGH is a rare presentation of HSV genital infection that has been described in immunocompromised patients7, especially in association with HIV infection6. The reason why this hypertrophic variant is more prevalent in HIV-positive patients is uncertain, as it appears to have no relation with CD4+ T lymphocyte count, nor with the immunosuppression5,8. Possible immunological mechanisms for the development of hypertrophic lesions include increased production of tumor necrosis factor -alpha by factor XIII-positive plamocytoid dendritic cells, promoting a growth of keratinocytes and consequent acanthosis and hyperkeratosis. Furthermore, the decreased production of interferon -gamma, which regulates the activity of keratinocytes, may also contribute to its development3,5.
This atypical manifestation is characterized by the presence of painful, well-defined exophytic masses with an irregular and ulcerated surface. The lesions are usually located in the perianal region, vulva, penis, and scrotum, but there are reports of similar extragenital lesions3,7.
The diagnosis depends on a high level of clinical suspicion with clinicopathological correlation, being fundamental for the exclusion of other infectious or non-infectious causes (genital condyloma and squamous cell carcinoma for example)6,7. Histopathology and virus identification support the diagnosis, but very small samples may be insufficient for diagnostic confirmation, due to the intense inflammatory response that can mask the diagnosis5. Histopathology shows a variable hyperplasia of the epidermis, with multinucleated epithelial cells and dense mixed inflammatory infiltrate composed of lymphocytes, plasma cells, and eosinophils. The identification of HSV in the lesion can be obtained by polymerase chain reaction or immunohistochemical methods9.
HSV infections in immune compromised patients should be treated with first-line systemic antivirals such as acyclovir (intravenous or oral) valacyclovir and famciclovir (foscanet and cidofovir can be used as a second-line treatment). However, atypical presentations of HSV infections, including HGH, are frequently resistant to antivirals. Thus, surgical excision may be considered, as in the present case8,10. A combined therapy of surgical excision with prophylactic antiretroviral drugs may also be an option. Finally, despite the lack of randomized studies, topical imiquimod and oral thalidomide have been described as an effective topical treatment for hypertrophic lesions in immunocompromised patients8,11,12.
Conclusion
HGH is a rare presentation of HSV genital infection, which must be included in the differential diagnosis of vegetating anogenital lesions in immunocompromised patients, especially in HIV infection. Biopsy is crucial to exclude other infectious and non-infectious causes. In the therapeutic approach, the likely resistance of this atypical form to antivirals must be considered, and additional topical imiquimod and surgical excision may be effective alternatives.