Introduction
Chagas disease is an endemic trypanosomiasis in South and Central America. Reactivation of chronic Chagas disease is a rare condition that exclusively occurs in immunosuppressed patients1. Skin involvement has been reported in patients with chronic Chagas disease following heart or kidney transplantation, leading to the reactivation of trypanosomiasis. Skin lesions typically manifest as rashes on the lower limbs and painful nodules that eventually progress to ulceration. Amastigote forms of Trypanosoma cruzi are consistently detected in the skin in all cases of cutaneous involvement commitment2.
Infective panniculitis refers to inflammations of the subcutaneous fat induced by various microorganisms. The immunosuppressed population is on the rise due to factors such as HIV infection, organ transplantation, and the widespread use of immunosuppressive drugs. This increase has led to a higher incidence of common skin infections, making opportunistic pathogen infections more prevalent and resulting in atypical presentations, including panniculitis3.
These cutaneous manifestations typically present in a non-specific manner within the immunosuppressed population. Presentation characteristics are strongly influenced by the virulence of the specific organism and the immune status of the host. Therefore, diagnosing panniculitis requires both microbiological and histological studies3.
Case report
A 51-year-old female patient with a history of cardiac transplantation due to Chagas disease and immunosuppression was admitted to the hospital due to acute myocardial cellular rejection. Her medical history included hypertension, chronic kidney disease, intermittent atrial fibrillation, and type 2 diabetes mellitus. She was being treated with mycophenolate sodium (720 mg every 12 h), cyclosporine (50 mg every 12 h), acetylsalicylic acid (100 mg once a day), atorvastatin (40 mg once a day), amiodarone (200 mg once a day), nifedipine (10 mg every 12 h), metformin (850 mg once a day), and rivaroxaban (100 mg once a day).
The patient underwent an elective endomyocardial biopsy due to complaints of worsening dyspnea, palpitations, and dry cough. She was hospitalized following the diagnosis of Grade 2R moderate acute cellular rejection (immunohistochemistry CDd negative, CD3 positive, CD20 positive, and CD68 positive).
However, during her hospital stay, she developed a daily fever. Infectious screening was conducted, and treatment with ganciclovir for cytomegalovirus was initiated due to positive test results, in addition to antibiotic therapy with ceftriaxone. Her condition continued to deteriorate, leading to pancytopenia and worsening of fever spikes.
After 30 days of hospitalization, the patient noticed painful erythematous nodules measuring between 2 and 4 cm on her legs, glutes, and lower abdomen (Fig. 1). The dermatology team was consulted, and they suspected panniculitis. A deep biopsy of the lesion in the posterior region of the left lower limb, involving the subcutaneous tissue, was performed using a 4-mm punch, and histopathological analysis was requested.
The dermatology team considered several diagnostic possibilities, including panniculitis of inflammatory or infectious origin, erythema nodosum secondary to medications or infections, erythema induratum, and vasculitis.
Initially, amastigote forms were observed in the histopathological analysis, suggesting the hypothesis of cutaneous leishmaniasis. However, after immunohistochemistry, the presence of T. cruzi was confirmed in skin and subcutaneous samples (Fig. 2), and polymerase chain reaction was positive for Chagas disease.
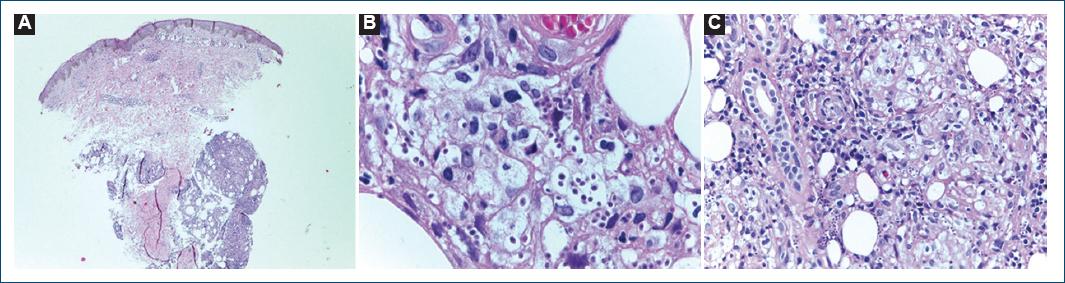
Figure 2 A-C: left gluteal biopsy. A: epidermis with foci of basal layer degeneration. The superficial and deep dermis exhibits perivascular lymphocytic inflammatory infiltrate. The hypodermis exudes an inflammatory infiltrate with a predominance of macrophages, presence of amastigote form of Trypanosoma cruzi and lobular panniculitis (H&E stain, magnification ×4). B and C: presence of amastigote form of T. cruzi and lobular panniculitis (H&E stain, magnification ×100).
During hospitalization due to Chagas disease reactivation, the patient was initially treated with corticosteroid pulse therapy (methylprednisolone, followed by prednisone), and following the diagnosis, she received benznidazole (100 mg every 12 h) for 60 days. In addition, she received immunosuppressive therapy due to her heart transplant, involving cyclosporine and sirolimus, as well as prophylaxis with antibiotics (bactrim, vancomycin, and teicoplanin) and antiviral medication (ganciclovir).
At present, the patient is under follow-up at the reference center, with no Chagas disease relapses following the established treatment and no further complications since the last hospitalization.
Given the rarity of the case, the cardiology, dermatology, and infectious disease teams were consulted for discussion, and it was decided to initiate treatment for the reactivation of Chagas disease. The patient showed improvement in the panniculitis after starting treatment.
Discussion
The case presented involves a patient who experienced an unusual manifestation of T. cruzi reactivation following immunosuppressive therapy. Reactivation of Chagas disease entails a transition from a latent or chronic state, in which the patient is stable, to an acute condition marked by increased parasitemia and serologic titers, leading to more severe lesions4. Typically, manifestations have been described as myocarditis, panniculitis, meningoencephalitis, and brain abscess, with myocarditis being the most frequent presentation5.
In immunosuppressed patients, the reactivation of Chagas disease can take on an atypical form, characterized by dermatologic symptoms and various skin lesions. These can include indurated erythematous plaques with necrosis in different areas, erythematous papules and nodules, skin ulcers, or panniculitidis4, as observed in the reported case.
In such cases, the amastigote forms of T. cruzi are not easily identified using common stains such as hematoxylin and eosin6. In some endemic areas, such as Brazil6,7, they must be differentiated from agents causing leishmaniasis, particularly in cases involving cutaneous lesions. Immunohistochemistry is a valuable tool for making this distinction, as was the case in our reported case, where this analysis enabled the correct diagnosis, especially after unsuccessful attempts to detect the parasite in peripheral blood and endomyocardial biopsy. Polymerase chain reaction was also crucial in confirming the recurrence of Chagas disease5.
The administration of antiparasitic treatment for symptomatic or oligosymptomatic patients with chronic Chagas disease is justified to attempt to eradicate the parasite. This is particularly important in infected patients who may later become organ donors or recipients of transplants and in those who, due to various causes of immunocompromised, may experience dissemination and/or acute infectious conditions4.
Despite its atypical presentation, the reported case underscores the importance of not disregarding such possibilities and emphasizes the need for histopathological and immunohistochemical analyses to complement the diagnostic process.















