Introduction
The erythrocyte sedimentation rate (ESR) is a laboratory test that measures the distance in millimeters that erythrocytes fall during one hour. Despite its ancient origins, dating back to the Greeks who observed the relationship between the sedimentation of red blood cells and fibrinogen (or "phlegma" as they called it), our understanding of the ESR has not substantially evolved. For both the Greeks and modern medicine, the rate of red cell sedimentation served as a means to detect the presence of specific bodily “humors".1
Widely regarded as a “marker of sickness",2,3the ESR, particularly extreme elevations of 100 mm/h or greater, is typically associated with diseases categorized into infection, autoimmune, malignancy, renal disease, or miscellaneous.3-5
While an initial Mayo Clinic study identified malignancy as the most common cause of an ESR greater than 100 mm/h,4 subsequent research consistently pointed to infectious diseases as the predominant category.6 As early as 1986, Fincher emphasized that the finding of an ESR of 100 mm/h or more should not trigger an exhaustive search for an occult malignant neoplasm.3 Nevertheless, and despite these findings, physicians continue to associate extremely elevated ESR of unknown cause with malignancy.7
The distribution of diagnostic categories in patients with an ESR above 100 mm/h exhibits wide variation, potentially influenced by differences in patient populations seeking care at various institutions or countries,3as well as individual patient characteristics such as sex, age, or setting. In Portugal, our knowledge on this issue is limited to a single study conducted nearly three decades ago.8
The aim of the current study was threefold: (1) to identify the causes of extreme ESR elevation (>100 mm/h) in a Portuguese population, (2) to assess the influence of sex, age, and patient setting (inpatient, outpatient, emergency room) on the relative contribution of each disease category, and (3) to determine the five-year survival of patients with an ESR above 100 mm/h.
Patients and Methods
This study conducted a retrospective chart review of all adult patients with an ESR of 100 mm/h or greater (indicating extreme ESR elevations) at Hospital do Espírito Santo - Évora (HESE) from January 1, 2008, to December 31, 2012. The selection of patients was based on ESR determinations performed at our hospital's clinical pathology department during this time frame. The study was approved by HESE’s review board and the need for informed consent was waived by this board.
HESE is the sole public hospital in the Évora district - a predominantly rural district with approximately 180 000 inhabitants, in Portugal.
One of the authors examined patient records to determine diagnoses associated with elevated ESR up to a year after the initial elevated value was identified. Manual reviews of electronic medical records included assessments of clinical notes, pathology reports, and radiology reports for the year following the initial extreme elevation in ESR. Diagnoses were retained if the provider specifically attributed a diagnosis to the elevated sedimentation rate, if the diagnosis was known in the literature to be associated with an elevated sedimentation rate, or if the reviewer believed the diagnosis was likely associated. As in more recent studies, if a patient had more than one associated diagnosis, each diagnosis was included. In cases of doubt, patient records were reviewed by another author. Categories were divided, as in previous studies, into infection, inflammatory/autoimmune, malignancy, renal disease, and unknown. A subset analysis evaluated specific diagnoses within each category, and the top five most frequent diagnoses from each category were determined.
Deaths were identified using the Portuguese Electronic Prescription System (PEM), where all patients with a previous death certificate are identified with their death date.
Descriptive summaries were reported as mean/SD for continuous variables and as frequency (percentage) for categorical variables. Two-sided chi-square tests (or Fisher’s exact tests when appropriate) were used to assess associations between each disease category and categorical variables. The Mann-Whitney test was used for continuous variables. The association between ESR and CRP level was assessed using the Pearson correlation coefficient. A log-rank test was run to determine if there were differences in the survival distribution for the different categories of disease. All tests were two-sided, and p values less than 0.05 were considered statistically significant. The analysis was performed using SPSS Statistics for Windows software, version 20.0 (IBM).
Results
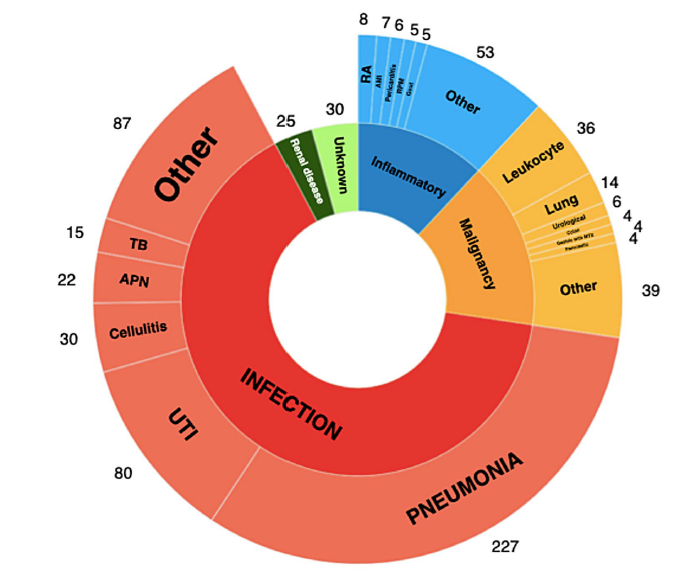
From January 1, 2008, to December 31, 2012, our hospital conducted a total of 72 439 ESR determinations, with 1069 (1.5%) showing levels of 100 mm/h or more, corresponding to 681 patients and 708 diagnoses. Among the patients in the study group, 355 (52.1%) were female, with a median age of 73 years (range, 1 to 99 years). Diagnoses were categorized as follows: infection (461, 65.1%), malignancy (107, 15.1%), inflammatory/autoimmune (85, 12.0%), unknown 30, 4.2%), and renal disease (25, 3.5%). Out of these diagnoses, 530 (75.9%) were from inpatients, 164 (23.2%) from outpatients, and 14 (2.0%) from patients in the emergency department.
The distribution of diagnoses varied significantly by patient setting. Outpatients had a higher prevalence of malignancy (31.7%) and inflammatory/autoimmune disease (23.8%), and much lower rates of infection (20.7%). Inpatients exhibited a higher prevalence of infection (78.9%) and lower frequencies in all other categories. All the above associations had statistical significance (p<0.001). The distribution in patients from the emergency department did not reach statistical significance.
Being female was associated with a slightly decreased frequency of malignancy (11.4%, p = 0.008). There were no statistically significant associations concerning sex and the frequency of the other diagnostic categories. Patients with inflammatory/autoimmune disease were younger (p = 0.001). The age of patients in the other diagnostic categories did not significantly differ from the overall group.
The most common diagnostic category was infection, with pneumonia being the most frequent subtype (227, 49.2%), followed by urinary tract infection (including pyelonephritis) (102, 22.1%), cellulitis (30, 6.5%), and tuberculosis (15, 3.3%), with several less frequent diagnoses accounting for the remaining 18.9%.
Malignancy was the second most common category, with leukocyte neoplasias (multiple myeloma, monoclonal gammopathy of undetermined significance, leukemia, and lymphoma) being the most frequent (36, 33.6%). This was followed, in descending order, by lung cancer (16, 15.0%), colorectal neoplasia (8, 7.5%), gastric cancer (7, 6.5%), and urothelial neoplasia (7, 6.5%), with several less frequent diagnoses accounting for the remaining 30.9%. Metastatic disease was present in 12.5% of lung cancer, 50% of colorectal neoplasia, 57.1% of gastric cancer, and 14.3% of urothelial neoplasia cases.
The third most common diagnostic category was inflammatory/autoimmune disease, encompassing various diseases with a broad distribution. Heart disease was the most frequent, with acute myocardial infarction, pericarditis, and Dressler syndrome (14, 16.5%). This was followed, in descending order, by rheumatoid arthritis (8, 9.4%), polymyalgia rheumatica (6, 7.1%), gout (5, 5.9%), and acute pancreatitis (5, 5.9%), with multiple less frequent diagnoses accounting for the remaining 55.2% (Table 1, Fig. 1).
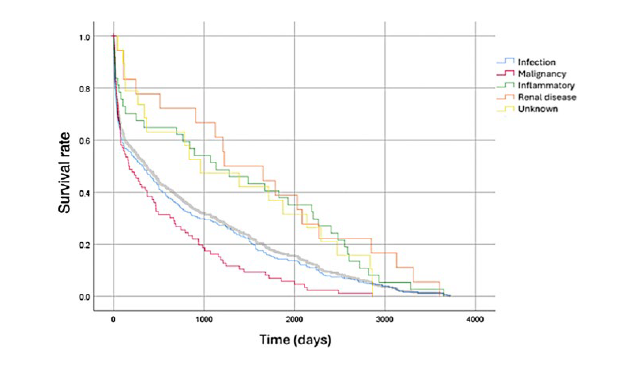
Five years after having an ESR above 100 mm/h, 479 patients had died (70.3%), with a mean time of 797 days (minimum 0 and maximum 3719, SD 960.9). A logrank test was run to determine if there were differences in the survival distribution for the different categories of disease. The survival distributions for malignant (χ2(1) =11.3, p = 0.001), inflammatory (χ2(1) =7.16, p = 0.007) and chronic kidney disease (χ2(1) =6.73, p = 0.009) were statistically significant when compared to overall survival. On the other hand, infection (χ2(1) =2.64, p = 0.104) and unknown diagnosis (χ2(1) =2.86, p = 0.09) failed to significantly differ from the overall survival curve. As such, mortality at 5 years was significantly increased for patients with malignancy (83%) and decreased for patients with inflammatory/autoimmune disease (45.9%) (Fig. 2).
A total of 650 of these patients also had a CRP value within 24 hours of an ESR value. In these patients, the Pearson correlation coefficients of ESR and CRP levels were not statistically significant (p = 0.149).
Discussion
In this study, an ESR above 100 mm/h was found in 1.5% of all ESR determinations. Infectious diseases constituted the most prevalent diagnostic category, observed in nearly two-thirds of our population, with pneumonia being the most common disease in almost one-third of all patients with an extreme elevation of ESR. The frequency of disease categories was significantly influenced by patient setting and sex. Malignancy was less frequent in women. Inpatients had a higher frequency of infection and less of all the other disease categories, with the opposite happening in outpatients. The five-year mortality rate was 70.3%, significantly higher in patients with malignancy and lower in patients with inflammatory/autoimmune disease.
Similar to previous research, we found that very few ESR determinations exceeded 100 mm/h (1.5% in our series, compared to 1% and 4.2% in other series2,3). Over 90% of patients had known diagnoses,2,3,6,9supporting the notion that extreme elevations in ESR are typically associated with an explanatory disease, serving as a "sickness index".2,3
Approximately two-thirds of our patients had infectious diseases (65.1%). Among the 16 studies reviewed by Daniels et al (6) from 1952 to 2017, infectious diseases were the most frequent diagnostic category in 14 studies, ranging from 25% to 92%. Pneumonia, consistent with previous research,5,6,10was the most common infectious disease in our population.
The percentages of patients with malignancy (15.1%) or inflammatory/autoimmune disease (12.0%) in our series fall within the broad range reported in other studies (malignancy 12%-58%, inflammatory/autoimmune diseases 3%-71%). The wide range in values across these series may reflect differences in patient populations seeking care at various institutions,3 as noted by Fincher in 1986, although methodological differences may also contribute. For instance, in our study, heart disease (acute myocardial infarction, pericarditis, and Dressler syndrome) and acute pancreatitis (without a diagnosis of infection) were included in the inflammatory/autoimmune disease category, representing 22.4% of this category. However, these diagnoses were absent in the largest study on this subject by Daniels et al.6
In our study, approximately half of the patients with gastric or colorectal cancer had metastasis, with a lower percentage of metastatic disease in cases of lung or urothelial neoplasia - a finding that diverges from the results of other authors, who considered that patients with a malignant cause for an extreme elevation of ESR would almost always have metastatic disease.3,9,11,12
In our population, infectious diseases were much less likely in outpatients (20.7% instead of 65.1%), as were malignant diseases in females (11.4% instead of 15.1%), and patients with inflammatory/autoimmune diseases were younger. We are not aware of other studies that found an association between age, sex, or setting, and the distribution of disease categories in patients with extreme elevations in ESR.
The patients in our series had a five-year mortality rate of 70.3%, surpassing usual rates for heart failure (67%13), cirrhosis (52.5%14), colorectal cancer (63%), breast cancer (91%), and prostate cancer (97%).15 We are aware of only another study with results on mortality and survival,9 although only short-term results were presented (mortality 12% at one month, and 34% at 6 months). Although in our study mortality was higher for patients with malignancy and lower for those with inflammatory/autoimmune disease, as expected, we were surprised to find that almost half of the latter died during this period: patients with an inflammatory/autoimmune disease and a ESR above 100 mm/h had a five-year mortality rate of 45.9%, in our population. We believe these results might have been influenced by the inclusion of heart disease and acute pancreatitis patients in this category, as stated above.
The correlation between the values of ESR and CRP did not reach statistical significance, a finding similar to previous research.6,16,17
This was a retrospective, single-institution study, which may limit generalization to other settings, in line with the above-mentioned statement by Fincher on “differences in the patient populations seeking care at the various institutions” and other differences in methodology. Nevertheless, and to our knowledge, the present study is the second-largest study of diagnoses associated with extreme elevations in ESR6 and the first one to present five-year mortality rates.
Conclusion
This study of patients with extreme ESR elevations, the second largest of its kind to date, reaffirms findings from previous research reporting that almost all patients have an identifiable etiology, that infection is the most common disease association, and that ESR and CRP levels correlate poorly in these patients. Unlike some previous studies, we found that, in patients with malignancy, an extreme elevation in ESR is not pathognomonic of metastatic disease. We also found that mortality at five years was 70.3%, higher in patients with malignancy (83%), and lower in patients with inflammatory/autoimmune disease (45.9%), findings that have not been previously described.
These findings may enhance the diagnostic and prognostic evaluation of patients with extreme elevations in ESR.