Background/introduction
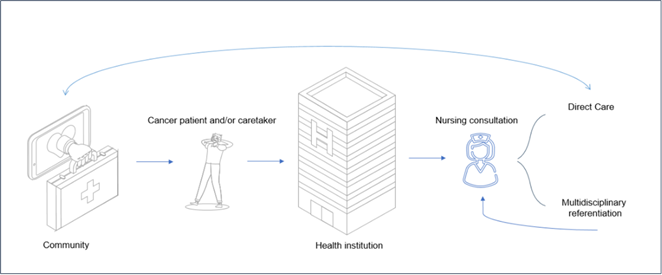
Percutaneous gastrostomy tube placement is a widely accepted method for providing long-term enteric nutrition and serves important health outcomes in adult and pediatric populations with cancer or neurologic diseases. 1-3 The implementation procedure, and its continuous care originate important health transitions, usually managed in medical appointments led by physicians. Generically, creating a radiologic percutaneous gastrostomy involves four sequential stages according to the availability of professionals and hospital resources: (1) hospital medical consultation for decision-making; (2) medical consultation for admission to hospitalization; (3) device implantation in a hybrid operating room (mixed team); (4) medical discharge to the community. After discharge, follow-up is determined by Portuguese health policies and most transitions are carried out by a physician, who also performs functions in the hybrid intervention room.4-6, therefore, the expansion of autonomous nursing interventions can help reduce the burden and optimize and integrate care. After implantation, the patient is under the care of the hospital team, with the frequency of care defined according to the nurse's clinical guidance and person-centred care principles.2,3,7 Nurse-led activities can improve outcomes, particularly quality of life, patient engagement, and patient satisfaction. 8,9 However, the economic impact of these activities is not well studied, although it does not appear to be detrimental.9,10 This fact raises doubts as to whether, in fact, care management for gastrostomy patients in the community is being carried out as efficiently and cost-effectively as possible. This article aims to present a business case pitch privileging nurse-led interventions regarding the care of the person with gastrostomy.
Development
The Business Case
A business case plan should provide stakeholders a structured proposal or framework for decision-making. Although not born in healthcare11,12 , in this context this approach to care planning might be a perfect way to approach the complexity of nursing transforming into quantifiable, evidence-based projects or objective proposals from a cost-benefit and quality point of view. 13-15 Not necessarily aiming to constitute a project in itself, the business case should overview objectives, costs and potential benefits or risks. It might be linked, if accepted, to a continuous improvement cycle such as “before”, “during” and “after implementation”. 16,17
The current business case thus intends to propose care exclusively led by nurses, supported by the nursing consultation methodology 18,19 and primary nurse work method.20 The med-surge specialist nurse will autonomously assume the interdependent dimensions of admission to hospitalization, discharge to the community and follow-up. Nurse-led methodology has already shown to be beneficial, in the pediatric community, and proximity and tailored care in gastrostomy patients has already been shown to be beneficial 21,22 The methodology is the visual presentation proposed by Osterwald e Pigneur - “Business Model Canvas”. 23
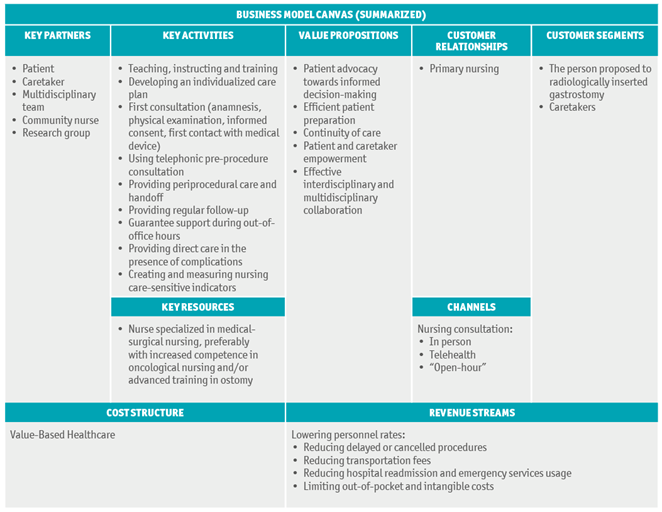
1. The customer segments
The customer segment represents the heart of any business case as it comprises the stakeholders that benefit from the model itself, preferably generating revenue. In this case, two important segments will benefit from implementing the proposed changes: people submitted to radiologically inserted gastrostomy as well as its’ caretakers when applicable. This model might also apply to endoscopic gastrostomy since the clinical pathway is similar. As referred before, this patient segment represents an important share of the total patients who use enteral feeding as their primary nutritional support and is a widely spread condition. 24-27 Special needs regarding this population are distributed through a series of incursions in the healthcare system each with different focus and goals. The prominent navigation landmarks include:
2. Value proposition
Value proposition encompasses the advantages if a particular model from the stakeholders’ perspective. As stated before, this model is directed to a unique population, prone to deficient continuity of care due to multiple contacts with the health system. In this nurse-led model, these contacts will be enriched with directed interventions towards patient and caretaker-centered needs. We believe an evolution away from a physician-centred care, will create value by improving the quality of care through:
- Assuring patient advocacy towards informed decision-making28;
- Ensuring correct beforehand patient preparation (regarding technical, health quality and security issues);
- Securing handoff and handout and reducing missed care29 (ensuring continuity of care);
- Encouraging self-care, self-management shown to be beneficial 30, and with potential improvement in quality of life 31 ;
- Promoting self-monitoring, management of complications when requested and beyond the scope of self-care 2,3,32;
- Conducting basic nutritional assessment 33;
- Evaluating the need for differentiated referral (nutrition, psychological, social worker, medical);
3. The channels
Channels constitute the means of communication used to provide a service. The channels planned to cover the needs of people with an ostomy are already found in any health institution. They are provided for in the legislation and statutes of regulatory bodies and do not require further financial investment. These include a nursing consultation in person, over the phone or via communication platforms 18,19,34. Additional support will be provided via email and short-messaging support groups, following telehealth, principals.35 Additionally, creating a monthly digital “open-hour” for all professionals who wish to be enlightened about gastrostomy care is advised.
4. Customer relationships
In a given business, the relationship with the customer can take different forms, depending on the characteristics of the customer service and goals to be achieved. In the particular case of ostomized patients and the management of their care, this relationship can become complex and expensive for the healthcare system. Therefore, the central methodology adopted for the relationship will be that of primary nursing. This nurse will serve all patients in this group and will be the entry hub into the healthcare system, creating objective and explicit reference interdisciplinary communication channels. The primary nursing methodology has proven to be beneficial not only to the patient 36 and caretaker but also the nurse. 30
5. Revenue streams (the financial case37):
In a business, revenue streams encompass the profit from the sale of a product. In health systems, particularly the portuguese, providing care is not always associated with direct payment. In Portugal, the health financing model used is based on the Beveridge model, making healthcare services available to all citizens on a payment basis taxes38 and moderating fees, which aim to prevent excess use and have a role in moderating healthcare consumption. 39 Thus, in the business case now exposed, although sustained by proximity care, we are not in a position to outline forms of direct financial profit, but rather a potential for cost reduction, related (in a non-exhaustive way) with:
- Lowering rates:
- Nurse-led consultation is cheaper by 40% than physician-led consultation, especially in the emergency room18;
- Nurse-led tube replacement in consultation room is approximately 80% cheaper when compared to the traditional hybrid room replacement;
- Reducing delayed or cancelled events related to factors like deficient or uncertain preparation40;
- Reducing patient and health system, transportation fees, using the documented benefits of telemedicine 41;
- Reducing hospital readmission and emergency services usage, due to inadequate patient empowerment and complications, such as local infection and leaking 22,35.
- Out-of-pocket and intangible costs.
6. Key resources
Key resources represent the assets and consequential value needed to achieve the proposed goals. The resources that are needed depend largely on the nature of the proposal. In healthcare, namely cancer care, the most expensive resource are cancer drugs. 42 Although this business case is exclusive to cancer patients, further investment is not related to drugs but mostly on human resources. Therefore, the only resource indispensable to respond to this new approach to care is a nurse specialized in medical-surgical nursing, preferably with increased competence in oncological nursing and/or advanced training in ostomy. All other necessary resources are expected to be pre-existing in a health institution equipped to implant a gastrostomy. Among these, the following stand out: a consultation office equipped as referred to in the supplementary material section, a mobile phone with an internet connection and clinical consumables related to specific management of the medical device.
7. Key activities
Key activities refer to the main actions or interventions stakeholders take to attain success. When dealing with patients, success is translated by positive outcomes (either patient-reported or professional-reported). Examples of positive outcomes in the gastrostomized patient are: undelayed and complication-free tube placement and management, patient and caretaker mastery regarding knowledge, ability and attitude (or volition) to manage the device, adherence to good practice and unfragmented continuity of care. Indeed, given the nature of care, the intention is to center key activities in the scope of practice of reference nurse. These will include nursing care aiding to facilitate the implementation of transition processes, as stated below:
- Enabling the person and significant caregiver to experience the minimally invasive procedure through teaching, instructing and training;
- Developing a care design plan according to the needs identified along the continuum:
- Conducting first consultation with cancer patient (anamnesis, physical examination, informed consent, first contact with medical device)33;
- Using telephonic pre-procedure consultation to review preparation (as stated in the supplementary material section)35;
- Providing evidence-based care activities during the periprocedural period, and securing correct and documented handoff to inpatient infirmary and community43;
- Ensuring first consultation 15 days after tube implantation and follow-up consultations according to patient needs and device characteristics during office hours2,3;
- Guarantee minimal support during out-of-office hours using digital communication channels35;
- Providing direct care in the presence of tube-related complications7;
- Creating and measuring nursing care-sensitive indicators, namely satisfaction with care, engagement level, capacitation, self-efficacy and quality of life.
8. Key partnerships
Care coordination and continuity ensure that all providers and organizations involved in health care provide the proper care at the right time, involving a people-centric approach. Although autonomous nurse-led follow-up has proven to be valuable44, multiple partnerships must be created to avoid gaps in care. The most important partnership will be created with the patient itself, based on the benefits of relationship continuity.45 Implementation and maintenance of the current nurse-led care will be reinforced by:
- Creating and publishing normative roles and responsibilities of all people involved in care, including the patient’s role in self-care;
- Presenting the new model of care beforehand to institutional stakeholders, including interventional radiology clinicians, nursing administration and representatives of the various interdisciplinary departments, including nutrition and surgical and medical wards;
- Promoting regular workshops among community and external institution nurses, empowering them to collaborate with care;
- Establish relationships with research groups to study and continuously improve care supported in evidence-based practice.
9. Cost structure
Costs must be reduced for all incursions into the health system since resources are finite. Although the nature of this business case focuses on an apparent reduction in funds spent, this is a reductive view of its overall value. Besides the initial investment in a specialized nurse, as referred to in “key resources”, there is no prediction of any costs increase. Consequently, it is important to note that, as in any other "healthcare business", the preferred outcomes will not necessarily focus on profit but rather on value-based care, a mixed approach that will not only seek to reduce as much as possible the expense associated with care but simultaneously provide the best possible outcomes for the person treated.46
Conclusion
Expanding specialized intervention nursing represents a strategic opportunity to improve clinical and financial indicators. The use of team elements with lower rate/ per hour worked, can provide sustainability to this model. However, the initial investment does not fit entirely into the current portuguese economic and legislative conjuncture. The main risks associated with this remoldingmight be related to resistance to change by stakeholders (perception of activity, confusion of roles), resistance by funders to the allocation of differentiated human resources (perceived value) and the absence or inadequacy of “nurse-led acts” in the current health regulations.