Introduction
Acute otitis media (AOM) is one of the most common infectious diseases in children, representing the principal cause of antibiotic prescription in the paediatric population 1-3.
Although the incidence of AOM related complications has decreased in the last decades, they remain clinically significant 4. Secondary facial nerve palsy (FNP) is one of the extracranial complications of AOM, affecting about 0,005% of patients with this condition 5.
The exact cause of FNP in AOM remains unclear. Several mechanisms have been proposed to explain this complication in patients with AOM assuming a bacterial origin 5-7. However, in about 1/3 of these patients no bacteria can be isolated from the middle ear 8. On the other hand, in some of sterile AOM, viruses can be detected in the middle ear exudate or acute viral infection can be serologically diagnosed 9. One of those viruses is Epstein-Barr virus (EBV), whose acute infection can cause neurologic complications in 0,5% to 7,5% of the patients 10.
In this work we present a case of FNP secondary to AOM caused by EBV infection in a child and review the few previously published case reports available in the literature on this subject.
Material and Methods
We conducted a review of the literature in december 2024 using PubMed (Medline), Scopus and Web of Science databases. On the former, the following query was used: "facial nerve palsy" AND ("acute otitis media" OR "otitis media") AND ("Epstein-Barr virus" OR "EBV"). Similar terms were used in the two other databases.
Case reports and case series were retrieved, and we further searched their references for other relevant publications.
There were only included articles written in English or Portuguese. Publications lacking clinical data were excluded.
Informed consent was obtained from our patient legal representative for publication purposes.
Case presentation
A 3-year-old previously healthy boy was admitted to the paediatric emergency department of a neighbour hospital because of a 12-hour history of facial asymmetry. He was on day two of oral antibiotic therapy with Amoxicillin + Clavulanic acid because of bilateral acute otitis media.
On admission he was apyretic and the remaining vital signs were normal. His general condition was good. He had a grade III right side peripheral facial palsy based on the House-Brackmann facial nerve grading system 11. The remaining neurologic examination was normal. Otoscopy revealed bilateral erythematous and bulging tympanic membranes suggestive of bilateral AOM. There was no auricle protrusion or retroauricular inflammatory signs.
The laboratory tests revealed no leucocytosis and no other abnormalities apart from a slightly elevated C-reactive protein (CRP) (5,6 mg/L - normal value <3,0 mg/ L).
It was assumed the diagnosis of AOM-induced right side facial nerve palsy and he was immediately started on intravenous antibiotic therapy with ceftriaxone 60 mg/kg/day and clindamycin (90 mg/kg/day) as also on intravenous (IV) methylprednisolone (10 mg/day). In the same day he had bilateral myringotomy with placement of ventilation tubes (VT) (Shepard ®). The middle ear was filled with purulent material which unfortunately was not sent for microbiology.
On the following day the patient was transferred to our hospital to complete antibiotic and corticoid therapy. He also initiated topic antibiotic therapy with Ofloxacin + Dexamethasone (1 mg/ml + 3 mg/ml) and started physical rehabilitation.
After 3 days of medical therapy, there was still no improvement of the facial nerve palsy. Otoscopy of the right ear revealed abundant purulent discharge and swelling of the posterior aspect of the external ear canal. Clinically, the patient was more irritable than usual and was refusing food, despite remaining apyretic.
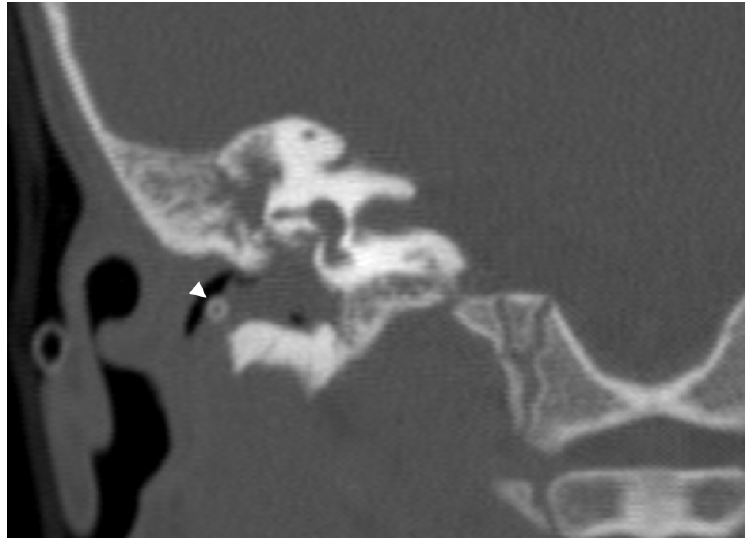
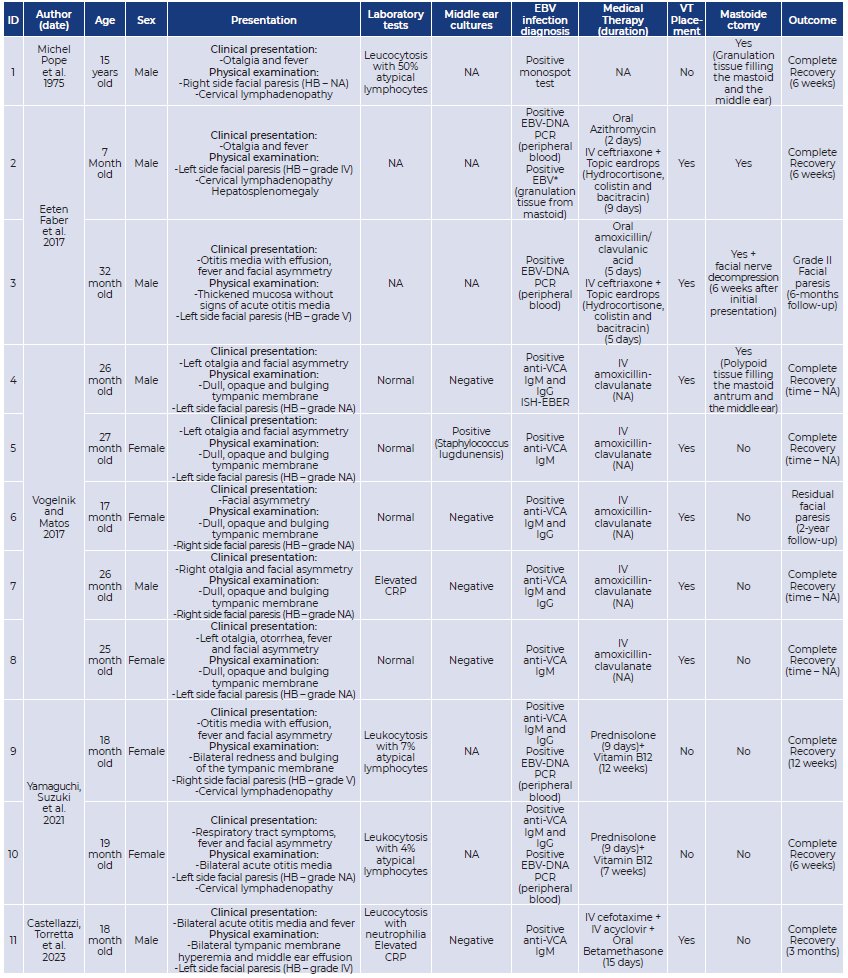
Figure 1 CT-scan of the right ear showing complete obliteration of the middle ear with soft tissue density material that protruded thought the tympanic membrane into the external ear canal displacing the ventilation tube (arrowhead).
A contrasted head CT-scan revealed complete opacification of the right mastoid and middle ear with soft tissue density material that protruded thought the tympanic membrane into the external ear canal displacing the ventilation tube (Figure 1). The ossicular chain was intact and there was no dehiscence of the tegmen tympani or of the tegmen mastoideum. The scutum was intact. The left tympanic membrane was thickened, and the ventilation tube was in the correct position. The ipsilateral middle ear and mastoid were aerated.
The patient was then submitted to right ear canal wall-up mastoidectomy. The middle ear, mastoid antrum and mastoid cavity were filled with highly friable, polypoid material which was carefully removed and sent for histology and microbiology. The ossicular chain and chorda tympani were preserved. The mastoidectomy cavity and middle ear were filled with Spongostan® and irrigated with ofloxacin. Samples of otorrhea collected in the beginning of surgery were sent for microbiology too.
Serologic tests were also performed. Positive antiviral capsid antigen (VCA) IgM and negative anti-VCA IgG serologies suggested a primary EBV infection. Therefore, we searched for Epstein-Barr virus-encoded small RNAs (EBERs) in the biopsied material.
The ear discharge was sterile. The histopathologic analysis of the biopsied material revealed an inflammatory infiltrate, and it was detected expression of EBER by in situ hybridization analysis.
We assumed the diagnosis of facial nerve palsy secondary to AOM caused by an acute EBV infection.
After 8 days of IV antibiotic therapy and weaning of corticoid therapy the patient was discharched home. He continued topic therapy with Ofloxacin + Dexamethasone (1 mg/ml + 3 mg/ml) for two more weeks.
Three months after the initial presentation, the facial palsy had completely resolved, and he had a normal otoscopy.
Results
After reviewing of the available literature, we selected a total of 6 articles. Only 5 publications were included in this review, after exclusion of one case report because it was written in German. Among the included ones, 2 were single case reports and 3 were small case series.
Discussion
1 Presentation
Despite being rare, facial nerve palsy is the most common cranial nerve pathology both in children and adults 12. The causes of facial nerve palsy can be divided between acquired and congenital. Among the acquired etiologies, idiopathic facial palsy (Bell’s palsy) is the most common 12,13. However, acquired dysfunction of the facial nerve may be secondary to trauma, neoplasms, and infections 12.
Although the widespread of antibiotic treatment of AOM decreased the incidence of complications, AOM remains the main infectious cause of peripheral facial palsy in children 13-15. When facial nerve palsy occurs in the context of an acute otitis media, it is usually assumed that it is secondary to bacterial infection. However, some of these cases not only fail to demonstrate clinical and laboratorial signs suggestive of a bacterial infection but also end up by having negative cultures from the middle ear 9,16. Besides that, in up to 1/3 of these cases, patients have viruses detected in the middle ear or have serologically confirmed viral infections 9. This suggests that some viruses, such as EBV, might be involved in the pathogenesis of AOM related facial nerve palsy 8.
EBV is a ubiquitous herpes family virus that is mainly transmitted through respiratory secretions during childhood 17,18 . Primary EBV infection presentation is diverse and depends on the age and immune status of the patient. In most cases it is asymptomatic or presents as a benign febrile viral upper respiratory infection. In older patients, namely in adolescents and young adults, primary infection typically presents as infectious mononucleosis (IM) (fever, pharyngitis, adenopathy, hepatosplenomegaly, and fatigue) 18,19 . Acute infection may also be associated with neurologic complications in a small percentage of cases 19,20 .
None of the 11 cases included in this work occurred in adults. The case reported by Michel et al., was of a 15-year-old adolescent whose presentation was infectious mononucleosis accompanied by peripheral facial palsy and acute otitis media21 . The median age of presentation of the patients of the remaining cases was of 22 months (minimum 7 and maximum 32 months). Our patient was 38 months old at the time of the initial presentation. In addition to facial asymmetry, most of those patients reported otalgia and fever. Besides otoscopic signs suggestive of AOM, 4 patients also had cervical lymphadenopathy and one had hepatosplenomegaly. All the patients whose facial palsy was graded according to House-Brackman scale had a grade superior to III. None of the patients had complete facial palsy (grade VI). Our patient had a grade III right side facial palsy.
2. Laboratorial findings
One of the typical laboratory findings of IM is the transient appearance of atypical lymphocytes 22. In fact, lymphocytosis and the presence of ≥10% of atypical lymphocytes are two of the Hoagland’s criteria for the diagnosis of IM 23. Nevertheless, despite their high specificity, the lack of sensitivity does not permit acute EBV-infection exclusion when they are not present. Elevated CRP is frequent in the acute EBV-infection24. Also, elevated levels of alanine aminotransferase (ALT), Aspartate Aminotransferase (AST) and lactate dehydrogenase (LDH) are commonly found in older patients. These findings are less frequently found in preschool children 24.
Only 3 of the patients had leukocytosis with the presence of atypical lymphocytes. In one case, the patient had leucocytosis with neutrophilia. Elevated CRP was present in 3 patients. 4 patients had normal blood cell counts and CRP. Our patient had leukocytosis with mildly elevated CRP. In none of the reported cases were mentioned liver enzyme levels.
Acute EBV infection gives rise to an immune response which generates specific and non-specific (heterophile) antibodies in the host. These heterophile antibodies (HA) are able to agglutinate animal erythrocytes, a characteristic that is behind Paul-Bunnell and Monospot tests22. Although these tests have high specificity, they are less sensitive than EBV-specific serologies 25. In fact, HA antibodies can be falsely negative in about 25% of patients within the first week and 6.5% of patients in the second week of IM 26. On the other hand, they can remain positive for as long as 1 year after the infection, requiring adequate clinical interpretation25. Specific EBV antibodies are directed against viral proteins produced in different phases of the infection22. VCA IgM antibodies are usually present 8 days before the onset of symptoms and last for 4 to 8 weeks. VCA IgG antibodies appear latter in the infection, but in some cases can be detected when the symptoms appear, persisting indefinitely25. Thereby, acute EBV infection can be serologically detected by isolated positive anti-VCA IgM antibodies or positive anti-VCA IgM and IgG antibodies22,25. Anti-EBV nuclear antigen (EBNA) IgG antibodies are only detected 2 months after the symptoms, and indicates past EBV infection25. It is important to mention that in about 9% of patients with IM, specific EBV serologies are negative. Therefore, in patients in whom acute EBV infection is highly suspected these serologies should be repeated 25.
EBV DNA can also be detected and quantified by Polymerase Chain Reaction (PCR) in peripheral blood samples. However, in the clinical setting of an acute EBV infection its role may be limited as a low number of EBV DNA copies may not be useful to distinguish between an acute infection and the presence of latently infected cells 25. EBV can also be identified in tissue samples by detecting EBV-encoded small RNA (EBER) positive cells by in-situ hybridization (ISH) (27.
In 8 of the 11 reported cases, specific EBV serologies were used to make the diagnosis of acute EBV infection. In 2 of these patients, EBV DNA was also detected by PCR in the peripheral blood. In one of the cases reported by Vogelnik and colleagues, EBER positive cells were identified using ISH in tissue samples from the material filling the mastoid antrum and the middle ear 8. In our patient, the diagnosis of EBV primary infection was made both with the serologies and the detection of EBER in samples of the granulation tissue from the middle ear and the mastoid.
3. Treatment
Most cases of AOM related complications are effectively treated with correct antibiotic therapy with or without ventilation tube placement. In case of AOM related facial nerve palsy, myringotomy with or without VT placement is usually recommended when the tympanic membrane is intact 6. Besides the therapeutic utility, this procedure also allows collection of samples of middle ear exudates for microbiological analysis. Corticosteroid use in facial palsy may help reducing time of recovery by reducing the facial nerve inflammation and edema 6,28,29. The role of antivirals in the treatment of facial palsy without AOM is uncertain (30. Even in the cases of acute EBV infection there was no demonstrable benefit in the use of acyclovir 31.
Upon the diagnosis of peripheral facial palsy associated to AOM most patients of the reviewed cases started immediately IV antibiotic treatment. The cases reported by Eaten et al. were given oral antibiotic treatment initially, but switched to IV after few days. Those patients also started topic eardrops of antibiotic and corticosteroid 28. One patient also started IV acyclovir and oral betamethasone treatment 6. Only the cases reported by Yamaguchi and colleagues did not receive any antibiotic treatment. Instead, those patients started oral prednisolone and Vitamin B12 29. Among the 11 reviewed cases, only three patients did not have VT placed. Our patient was given IV ceftriaxone and clindamycin and IV methylprednisolone. He also started topic eardrops containing antibiotic and corticosteroids after VT placement.
In the setting of facial nerve palsy secondary to AOM, mastoidectomy is usually reserved for patients who experiment clinical worsening or that fail to improve after 7 days of adequate antibiotic treatment. In these cases, temporal bone CT scan is usually performed to search for signs of coalescent mastoiditis indicating the need for surgery 32,33. Surgical decompression of the facial nerve is not recommended in an early stage because the inflammation of the nerve increases the risk of damaging it 33. This procedure is usually reserved for patients with complete facial nerve palsy who have > 95% degeneration documented on Electroneuronography (between the 4th and the 14th days after the initial presentation) 34.
Only 4 of the reviewed cases were subjected to mastoidectomy. The rationale behind the decision to perform mastoidectomy in the case one reported by Vogelnik and colleagues was not revealed 8. In the cases reported by Eeten et al. one had mastoidectomy 6 days after the initial presentation after no demonstrable improvement with the antibiotic treatment and the other had mastoidectomy and facial nerve canal decompression after no improvement of the facial nerve palsy after 6 weeks 28. Our patient had mastoidectomy on day 4 of presentation after no improvement of the facial asymmetry and worsening of the general condition and of the otoscopy findings.
4. Prognosis
In all but one of the reported cases there was a complete recovery of the facial nerve palsy. The patient that did not have complete recovery still had a significant improvement. Our patient also had a complete recovery.
The good outcomes of the cases reported in this work are in accordance with the previously described favorable prognosis of facial nerve palsy secondary to AOM 6,28. As previously mentioned, the therapeutic strategies reported in the reviewed cases were significantly different from each other’s. This applies not only to the pharmacological treatment, but also to the surgical treatment. Despite that, all the patients had full or significant recovery. This makes it more difficult to draw conclusions about the treatment of this condition. Even in the patients who had mastoidectomy there is no evidence that the palsy was not going to resolve if surgery had not been performed.
Conclusion
The authors of this work suggest considering EBV primary infection in all cases of facial nerve palsy secondary to AOM, mainly in those cases who fail to demonstrate typical findings of bacterial infection. All these patients should be started on IV antibiotics and corticosteroids immediately and have myringotomy with VT placement and middle ear cultures. EBV specific serologies should also be performed in all patients. Mastoidectomy can be considered in some patients who fail to improve or experience worsening of the symptoms, however, there is no clear indication that it causes a significant change in the prognosis.
List of abbreviations:
ALT: Alanine aminotransferase
AOM: Acute otitis media
AST: Aspartate Aminotransferase
CRP: C Reactive Protein
EBERs: Epstein-Barr virus-encoded small RNAs
EBNA: Anti-EBV nuclear antigen
EBV: Epstein-Barr virus
FNP: Facial nerve palsy
HA: Heterophile antibodies
IM: Infectious mononucleosis
ISH: In-situ hybridization
IV: Intravenous
LDH: Lactate dehydrogenase
PCR: Polymerase Chain Reaction
VCA: Antiviral capsid antigen
VT: ventilation tube