Introduction
Osteomyelitis pubis is a rare condition that can occur after vaginal delivery and is associated with destruction of the bone and, frequently, the joint1. Obstetric injuries and abortion are known risk factors for this condition, as they can predispose to bacteremia and hematogenous infection of the pubic symphysis2. The most common pathogens involved are Staphylococcus Aureus and Pseudomonas Aeruginosa3.
The most common symptoms are pubic pain, painful gait and hip movements and fever that usually begin in the early post-partum period. Those, associated with inflammatory changes in laboratory and imaging exams plus positive blood cultures support the diagnosis4.
On this report we present a rare case of osteomyelitis pubis following an uncomplicated vaginal delivery. The authors required prior approval by the Ethics Committee of Hospital Garcia de Orta and requested informed consent from the respective patient.
Case presentation
A 24-year-old primipara was admitted to the hospital at 40 weeks of gestation with active labor. She had no pathological personal history and had an uncomplicated pregnancy with a negative swab for Group B Streptococcus at 36 weeks. After six hours of labor without complications, she had a normal delivery of a healthy newborn male with 2500 g, without perineal tears. Two days after the delivery she was discharged denying any symptoms.
However, on the day after, she presented to the emergency room with acute pain in pubic symphysis with irradiation to the groin and hip, which prevented her to stand or walk. On physical exam, she had low grade fever (38,4ºC), tenderness on lower abdomen and unremarkable gynecological observation. Blood tests revealed elevated C-reactive protein (CRP) (15 mg/dL) and sedimentation rate (102 sec), even though normal white blood cells count. Pelvic ultrasound was normal, as well as the pelvic x-ray that didn’t show any abnormal widening of the pubic symphysis.
At this time, a puerperal endometritis was suspected so blood cultures were performed, and intravenous Clindamycin (900 mg every 8 hours) plus Gentamicin (5 mg/kg/day) were started. Although fever remission, high CRP and pain persisted, and it was now more located to the pubic bone with irradiation to the right hip and any active or passive movement of the right hip evoked intense pain (specially with flexion and abduction).
For this reason, a computed tomography (CT) was performed and showed pre-pubic soft tissues higher density and intra-articular air in the symphysis pubis (Figure 1), which led to suspicion of an osteitis. A magnetic resonance imaging (MRI) confirmed the diagnosis by showing hyperintense T2 signal and cortical irregularities on the articular surface associated with few intra-articular fluid and densifications of the soft tissues (Figures 2 and 3). At the same time, blood cultures were positive for Streptoccocus Anginosus and a puerperal osteomyelitis pubis was assumed. Antibiotic therapy was changed to intravenous benzylpenicillin (24 million Units per day), according to the antibiogram. Considering the high diagnostic certainty, based on clinical and imagological features, and technical difficulties, an aspirative biopsy was not performed. In consideration to Streptoccocus Anginosus found on blood cultures, the patient was submitted to an echocardiogram that excluded any sign of endocarditis.
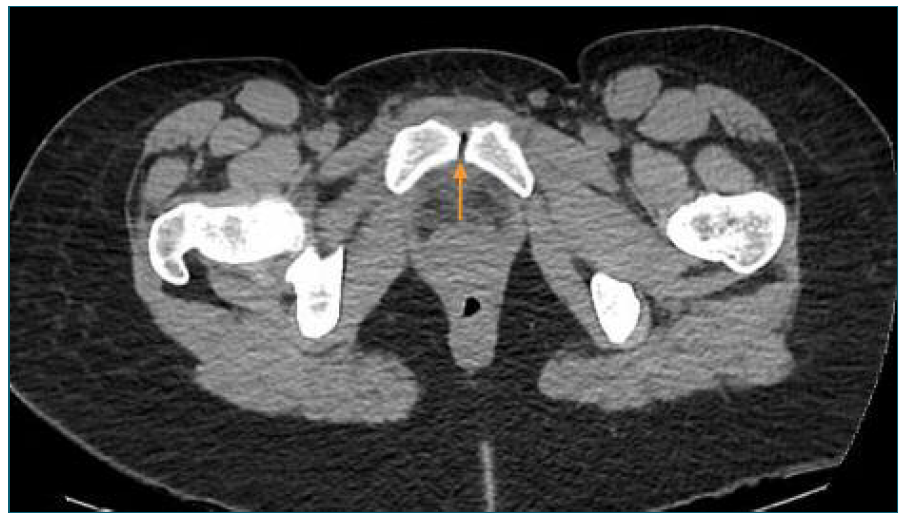
Figure 1 Pelvic CT scan. CT scan demonstrating intra-articular air and high density of soft tissues.
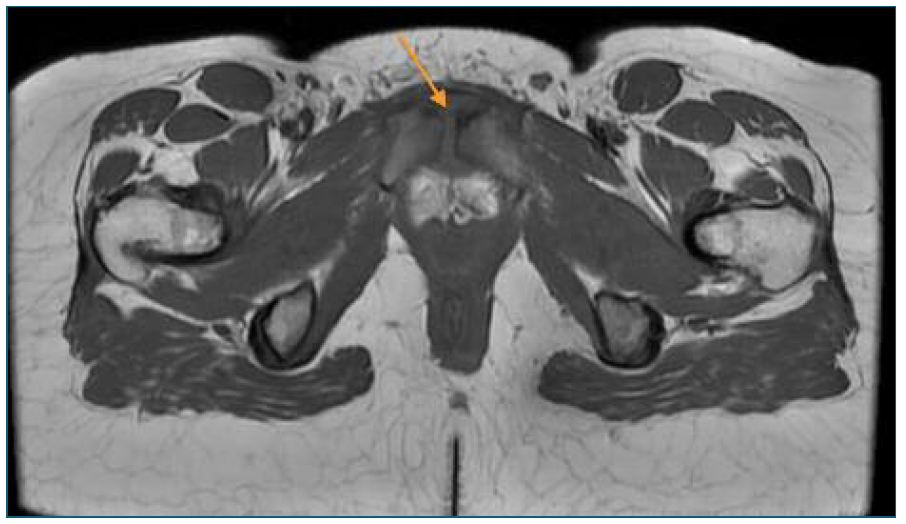
Figure 2 Pelvic MRI (axial plane) - MRI showing hyperintense T2 signal and cortical irregularities on the articular surface and densifications of the soft tissues.
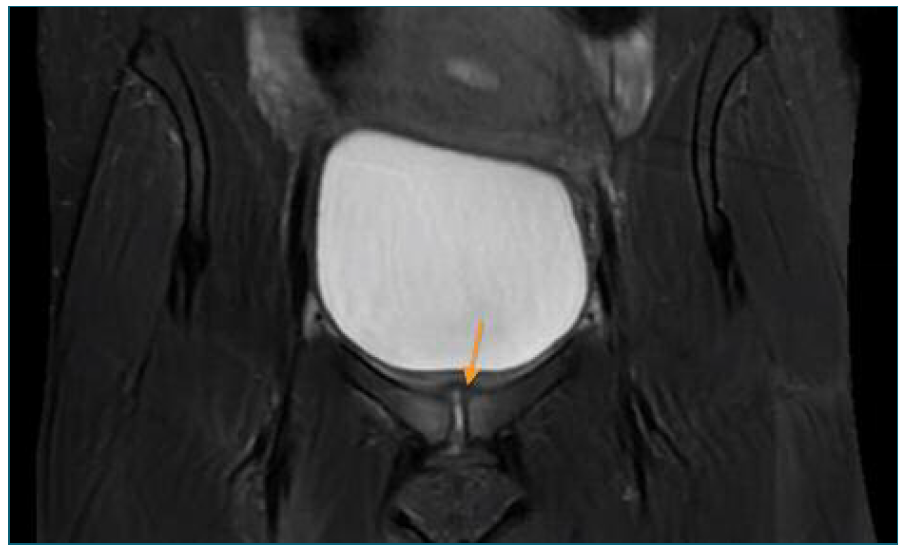
Figure 3 Pelvic MRI (coronal plane) - MRI showing hyperintense T2 signal and cortical irregularities on the articular surface and densifications of the soft tissues.
The patient improved few days after the new treatment and was discharged 1 week later. She continued intravenous treatment in a home hospitalization regimen for 4 weeks and for more 2 weeks with oral amoxicillin (1 g every 8 hours). In total, she completed 6 weeks of treatment until normal sedimentation rate was verified. Clinical evolution was good with remission of pain and one month after the end of treatment she had no recurrences or sequelae.
Discussion
Osteomyelitis pubis is a rare condition with a post-partum incidence of 0,01%1. There are few cases reported, mostly associated with normal vaginal deliveries1-11. Bacteremia was reported in 73% of cases of osteomyelitis pubis and most common pathogen is Staphylococcus Aureus, but P. aeruginosa and polymicrobial infections evolving fecal flora are also common3,12.
Urologic surgery, intra venous drug use, abortions and obstetric injuries are known risk factors2. In the largest cohort study of puerperal septic sypmphysitis, done in a tertiary hospital in Sweden, primiparity and vaginal instrumental delivery were recognized as risk factors for this condition, as those are associated to more frequent and serious perineal tears1.
The diagnosis is difficult as it can be confounded with pubic osteitis, a sterile inflammatory and self-limiting condition, or with other more frequent post-partum complications associated with pelvic pain, such as endometritis. A normal gynecological examination and ultrasound, associated with pelvic pain that worsens with movement plus high inflammatory markers and positive blood cultures should raise the suspicion of pubic osteomyelitis4. In some cases, fever may not be present and there may be a long period between the precipitating event and the onset of symptoms. A normal pelvic radiograph does not exclude the diagnosis, as the most sensitive imaging exam is MRI showing mostly bony destructions and fluid within the symphysis2.
Prompt initiation of antibiotic treatment is crucial for favorable clinical evolution. The choice of antibiotics should be preferably guided by culture of bone biopsy or pus obtained by percutaneous aspiration. When microbiology exams are not available, empiric antibiotics should cover Staphylococcus, gram-negative bacilli, and anaerobes. A rational initial regimen must include vancomycin and a third-generation cephalosporin plus metronidazole. Antibiotic therapy must be continued for at least 4 to 6 weeks and until erythrocyte sedimentation rate is normalized13,14. Surgical debridement or curettage is indicated in severe complications, such as bone necrosis, or symptoms not responding to antibiotic therapy5-8,14. In all cases reported the outcome was excellent after antibiotherapy was started, with no reports of long-term complications.
In conclusion, although pelvic trauma has been associated with osteomyelitis pubis, we present a case of osteomyelitis pubis related to uncomplicated vaginal delivery following a labor with normal progression. This condition is easily mistaken with more common puerperal complications, such as pubic osteitis or other pelvic inflammatory diseases. Fever, normal gynecologic examination, and location of pain should raise clinical suspicion. Clinicians must be aware of this diagnosis since pelvic surgery and labor are important risk factors. Prompt initiation of treatment is crucial for favorable clinical evolution.
Authors’ contributions
Mariana G. d’Almeida; Helena Cunha e Carmo and Cristina Leite: Contributed to the diagnosis of the clinical case, interpretation of data, critical review and final approval of the submitted version. Inês Neves Gomes; João Pedro Pereira: Contributed to the revision of literature and critical review of the article.














