Introduction
Percutaneous endoscopic gastrostomy (PEG) should be considered a first-line technique for long-term enteral feeding. This option is not definitive, and if the tube is removed the gastrocutaneous tract is expected to start healing within 24 h. Nonetheless, in some patients the tract fails to heal and the gastrocutaneous fistula persists. Endoscopic management is nowadays considered the first-line step in these cases. Through-the-scope (TTSC) or over-the-scope clips, argon plasma coagulation (APC) or even endoscopy-assisted suturing are options in avoiding surgical intervention in these fragile patients [1, 2]. The authors present 2 cases with chronic and refractory gasrocutaneous fistulas, after removal of PEG tubes, in which a different endoscopic approach was attempted.
Case 1
An 82-year-old woman, with enteral tube feeding due to amyotrophic lateral sclerosis since October 2020, was hospitalized for peristomal leakage 1 year later. Analytically, there were no relevant abnormalities. Her 24-Fr PEG tube was removed, the fistula borders were endoscopically cauterized by APC and the fistula partially closed with 3 TTSC. A 20-Fr PEG tube was placed but, 1 month later, we opted for permanent removal due to maintained peristomal drainage. Two weeks later the fistula persisted, so we proceeded with closure with an adapted tulip-bundle technique. The fistula edges were cauterized by APC, at 1.5L/min 50W, and an Endoloop® was positioned, anchored to the bordering normal mucosa, with five 11 mm TTSC, as seen in Figure 1a and b. The Endoloop® was tightened, with adequate endoscopic closure (shown in Fig. 1c). No procedure-related complications were reported. The patient passed away in April 2022 without fistula recurrence.
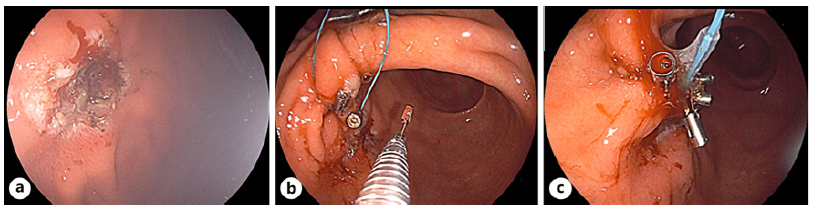
Fig. 1 Endoscopic closure of a chronic and refractory gastrocutaneous fistula in an 82-year-old woman. a Cauterization by APC of the defect borders. b After Endoloop® introduction and positioning, 5 TTSC were required and anchored in the adjacent normal mucosa. c Endoscopic closure of the defect after Endoloop® tightening.
Case 2
A 42-year-old quadriplegic man, under PEG tube feeding since June2015, was first admitted for abdominal wall cellulitis in September 2021, as seen in Figure 2. At admission, hemoglobin, albumin, and natremia were low (10.3 g/dL, 2.8 g/dL, and 135 mmol/L, respectively). His 24-Fr feeding tube was removed, a guidewire was positioned in its place, and antibiotics were started. As drainage persisted, we opted for endoscopic treatment. The fistula edges were cauterized by APC, at 1.5L/min 50W, before an over-the-score clips was positioned. Although with initial success, 2 months later the fistula reoccurred and a new endoscopy attempt was performed with 8 TTSC. An unsuccessful attempt to use the tulip-bundle technique was made, with Endoloop® failure. Five months later drainage persisted, and endoscopic treatment with tulip-bundle technique was proposed. Following cauterization of the edges, an Endoloop® was anchored to the mucosa bordering the defect using six 11 mm TTSC. The Endoloop® was tightened and closed the fistula edges, as illustrated in Figure 3a-c. This procedure was uneventful, and the patient was discharged with successful fistula closure. Unfortunately, 1 year later, probably due to patient’s intrinsic frailty, the fistula recurred, and surgical repair was deemed necessary.

Fig. 3 Endoscopic closure of the second chronic and refractory gastrocutaneous fistula described. a and b: Cauterization by APC of the defect borders. c The Endoloop® was positioned using 6 TTSC and tightened, successfully closing the fistula.
Only a handful of cases using the endoscopic tulip-bundle technique for closure of chronic gastrocutaneous fistulas have been described so far [3, 4]. Even so, it is an efficient and safe nonsurgical option, particularly helpful in high-risk patients. One could argue its role as an early approach for gastrocutaneous fistulas in the hope of reducing recurrence.















