Introduction
The development of a uretero-arterial fistula (UAF) is a rare and life-threatening condition. Owing to its low prevalence, diagnosis and management remains a challenge for both urologists and vascular surgeons and its high mortality rates (7-23%)1,2 may be at least partially attributed to delayed diagnosis.2 Despite being a rare cause of gross haematuria, its incidence has been increasing over the years making its recognition cornerstone for a successful treatment.3 Treatment options vary greatly but stent graft placement has been a recent, effective, and safe technique which allows the rapid resolution of haematuria.4
The purpose of this case report is to raise awareness of this entity among both vascular surgeons and urologists. We present a case of UAF in a patient with previous pelvic surgery and indwelling ureter catheter.
Clinical case
An 82-year-old male presented to the emergency department (ED) with haemodynamic instability and gross haematuria that started one hour prior to admission.
The patient had a medical history of hypertension, atrial fibrillation (under anticoagulation with dabigatran), and aortic valve stenosis. He had been submitted to a radical cystoprostatectomy and cutaneous ureterostomy for a vesical neoplasm 4-month prior to admission.
Objectively, at admission on the ED, patient was tachycardic, polypneic and hypotensive. The cutaneous ureterostomy was actively bleeding with arterial blood, and the collection pouch had about 1L grossly hematic urine.
The laboratory analysis revealed an acute anaemia with a haemoglobin of 7.5g/dl and worsened renal function with a serum creatine of 2.10 mg/dl (from a baseline of 1.2mg/dl). Blood coagulation tests showed and international normalized ratio of 1.2 with normal activated partial thromboplastin clotting time and slightly prolonged prothrombin time of 16s (normal range between 11.5-14.5s).
An urgent contrast enhanced computed tomography (CTA) was requested (figure 1 and figure 2). The arterial phase showed filling of the excretion system of the left kidney with hematic content, as well as ureterohydronephrosis; no acute findings were appreciated on the right kidney and excretory system. The exam also showed a subtle contrast blush adjacent to the inferior aspect of the left ureteral stent in intersecting area with the right common iliac artery.
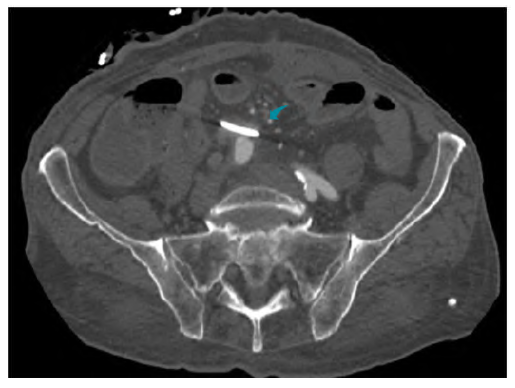
Figure 1 Axial view of CTA showing area of contact between stented left ureter (blue arrow) and right common iliac artery.
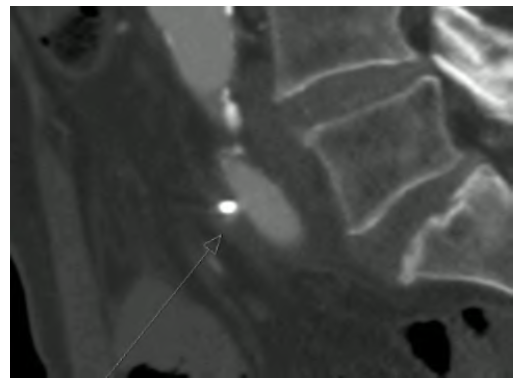
Figure 2 Sagittal view of CTA showing area of contact between stented left ureter (blue arrow) and right common iliac artery.
The patient was then taken to the angiography suit. Images obtained showed no identifiable contrast blush and therefore the fistula was not identified. Nonetheless, a balloon-expandable stent graft was deployed (GORE® VIABAHN® VBX - 11mm diameter and 59mm in length) at the intersecting point of the right common iliac artery and the stented left ureter (Figure 3).
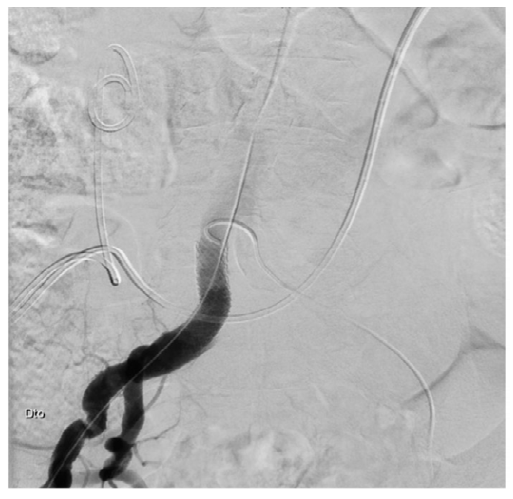
Figure 3 Angiographical image showing placed stent-graft in the right common iliac artery and its intimal relation with the left stented ureter.
Following the procedure, the haematuria resolved, and the patient had an uneventful post-operative stay. A new CTA scan was ordered at 72h hours post-op and showed no signs of early complications.
He was discharged two-weeks after admission, following a course of large spectrum antibiotic therapy, due to concerns over secondary infection. The decision to halt systemic anticoagulation was made based on a multidisciplinary meeting, maintaining single antiplatelet therapy.
The patient remained asymptomatic at 3 month follow up. The kidney function recovered to that prior to this event and haemoglobin rose spontaneously to 9.5mg/dl.
Discussion
Uretero-arterial fistula was deemed as a rare cause of haematuria. However, in recent years, its prevalence has been increasing, at least in part due to improvement in pelvic cancer treatment and due to increasing number of patients submitted to chronic ureteral stenting.5,6
UAF’s can be classified into primary (15%) - seen in aortoiliac aneurysmal disease - and secondary (85%) - that occur after pelvic surgery, vascular surgery, radiation therapy, or ureteral stenting.4
The main risk factors for the development of an UAF are chronic ureteral stenting, abdominal/ pelvic surgery, pelvic radiotherapy, and iliac artery aneurysms.2,7,8 History of pelvic neoplasm constitutes an important risk factor and cervical cancer appears to have the highest risk of development of UAF.3
The pathophysiology remains unclear. Under normal circumstances, the pulsatile arterial movement cause no harm to the ureter since the latter moves freely. Injury to the ureter or arterial wall (caused by indwelling catheter, previous surgery, or radiation therapy) may induce fibrosis and consequently lead to the fixation of the ureter to the adjacent vessel in its crossing point. In turn, this fixation could induce friction (due to the pulsatile movements of the artery) and cause focal necrosis, leading to the UAF.3,5
The most commonly afflicted vessel is the common iliac artery albeit cases have been described involving the external and internal iliac artery.1
The main symptom (and sometimes the only one) is gross haematuria which can be intermittent or persistent and up to 21% of patients will present with haemodynamic instability.1,2 Because of the intermittent nature of the symptoms, diagnosis can be easily missed and delayed and is also the reason that imaging methods have a very limited accuracy.5 In the majority of cases, CTAs show no identifiable abnormality , and only about a third of patients will present with pseudoaneurysms at fistula site, presence of blood clots in the excretory system, or hydronephrosis.5,6 The most sensitive exam seems to be selective iliac arteriography, nonetheless, with a sensitivity of only approximately 50%, however allowing a possible treatment.2,5
Surgical intervention in patients with UAF is often difficult due to hemodynamic instability and hostile abdomen from prior surgery and/or radiotherapy.2 Endovascular treatment seems an effective and less invasive modality particularly useful in controlling the arterial bleeding.2,7) Most reported cases report the use of either self-expandable or balloon-expandable stent grafts.9 Despite high primary technical success rates of endovascular treatment, up to 60% of patients will require open conversion due to recurrent bleeding, stent-graft infections, or other infectious complications (such as abscess formation).2,7,9
In patients requiring open surgery, several techniques have been described. In cases of proved infection, some authors suggest the use of femoral-femoral crossover bypass and iliac artery exclusion as this treatment modality avoids further manipulation of infected field.10
To date it is not known whether open surgical techniques are superior to endovascular in terms of long-term outcomes for this rare pathology.1
Conclusion
UAF should be included in the differential diagnosis of patients with unexplained haematuria who have a history of chronic ureteral stenting, pelvic surgery, aneurysm repair surgery or radiotherapy. Furthermore, it seems reasonable to perform a diagnostic angiography in the operating room or angiographic suite in patients with risk factors and a convincing medical history even if other imaging methods show no evidence of UAF.
Endovascular treatment with stent-grafts has become the mainstay in the management of UAF as it provides a minimally invasive alternative to open surgery, with lower morbidity rates. Endovascular treatment could also be perceived as a “bridge” to definitive treatment for unstable patients.















