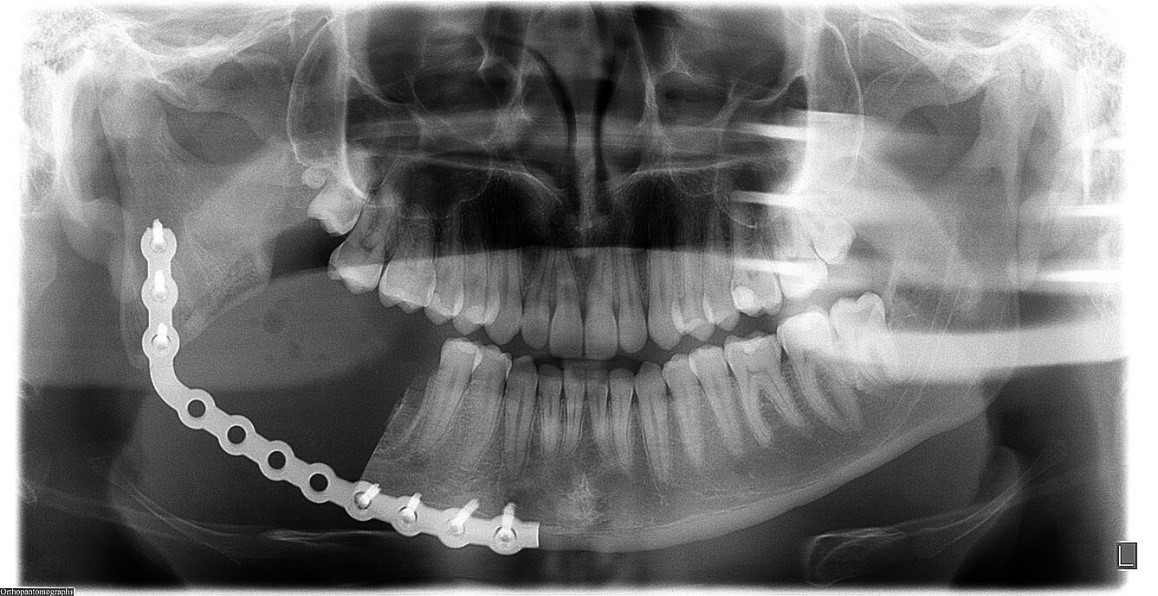
A 23-year-old male patient, black, attended the outpatient clinic due to volumetric increase in the right mandibular region, with a tumoral appearance, painless on palpation and without sensory impairment. The panoramic radiographic examination (Figure 1) showed a region with a mixed appearance, measuring approximately 5 cm, mainly affecting the periapical region of the lower second molar and the diagnostic hypotheses raised were bone dysplasia, cementoblastoma and osteoblastoma. Initially, an incisional biopsy was performed to confirm the diagnosis, which indicated the lesion as being cementoblastoma. After confirming the diagnosis, a computed tomography (Figure 2, A and B) was performed to better assess the dimensions and location of the lesion, for more accurate jaw surgical planning in the areas of 46 and 47 and in proximity to 48.
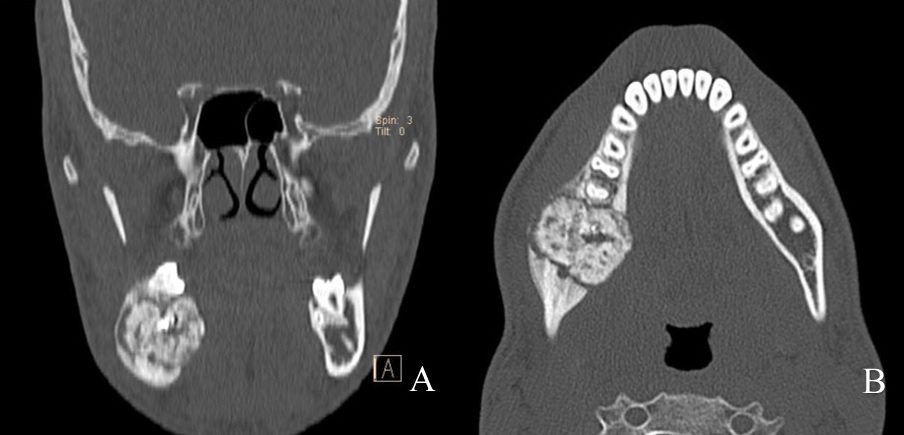
Figure 2: A- Axial bone window computed tomography scan showing the mandibular lesion in its anteroposterior and lateral dimensions. B- Coronal reformatted computed tomography image showing craniocaudal as well as lateral dimensions of the lesion.
The patient underwent segmental resection of the mandible, under general anesthesia, with installation of a 2.4mm Load Bearing fixation system to maintain stability, adequate mandibular contour and union of bone stumps (Figure 3).
Cementoblastoma has been updated and included in the 2017 WHO Classification of Odontogenic Tumors and is considered the only true neoplasm of cementum. This lesion affects most commonly the mandibular teeth (79.5%) and permanent mandibular first molars are the most common teeth involved1,2. The main characteristics of this usually asymptomatic tumor are its slow and unlimited growth, causing bone expansion without cortical destruction and facial asymmetry and, in very rare cases, lower lip paresthesia2,3.
This is frequently a casual radiographic finding and presentation depends on the stage of its maturation. The treatment of choice is complete surgical removal of the lesion with extraction of the tooth or associated teeth, and a conservative approach can be adopted through curettage and peripheral ostectomy, a technique recommended for small lesions1,2,3.
A more radical surgical approach, through resection, whether marginal or segmental, has been shown to be the best alternative with lower and minimal recurrence. The recurrence rate varies from 5.9% to 37.1%, either aggressive or conservative surgical treatment are adopted, respectively3.
Considering the recurrence variability depending on the treatment used, a long-term follow-up is essential, especially in cases where a so-called more conservative treatment is used.




![PET com 2-[18F]-FDG no Diagnóstico Diferencial entre Doença de Alzheimer e Demência Frontotemporal](/img/pt/prev.gif)