Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.23 no.5 Lisboa out. 2016
https://doi.org/10.1016/j.jpge.2016.01.005
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
Colonic Intussusception Caused by Colonic Lipoma
Invaginação Cólica Causada por Lipoma do Cólon
Filipa Ávila * , José Renato Pereira, Maria Antónia Duarte
Gastroenterology Department, Hospital do Divino Espirito Santo de Ponta Delgada, Ponta Delgada, Portugal
* Corresponding author.
Keywords: Colonic Diseases. Colonic Neoplasms. Intussusception/etiology. Lipoma/complications.
Palavras-chave: Doenças do Cólon. Neoplasias do Colón. Invaginação/etiologia. Lipoma/complicações.
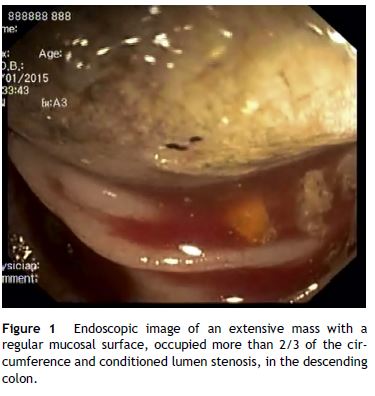
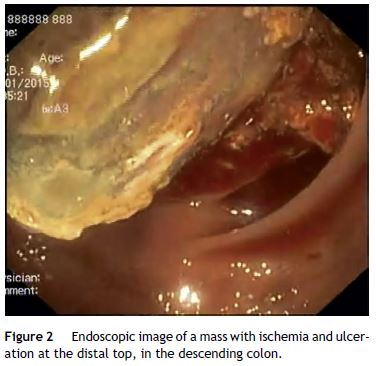
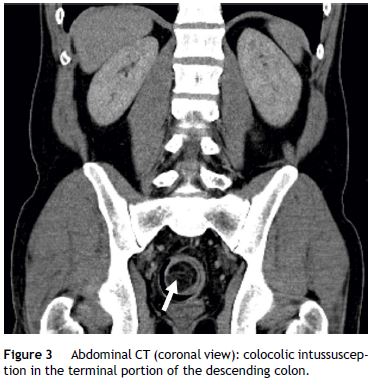
A 41-year-old man, was admitted in the emergency department due to repeated lower abdominal pain, constipation and hematochezia with one month of evolution. His past medical history was irrelevant. The physical examination and laboratory data were normal. The patient denied anorexia, weight loss and fever. A colonoscopy revealed an extensive mass with a regular mucosal surface with ischemia and ulceration at the distal top (Figs. 1 and 2), in the descending colon. This lesion occupied more than 2/3 of the circumference and conditioned lumen stenosis. Biopsies revealed inflammatory changes. An abdominal and pelvic computed tomography (CT) showed colocolic intussusception (Fig. 3), in the terminal portion of the descending colon, caused by a lipomatosus mass with 7 cm × 4 cm larger diameter (Fig. 4). The patient underwent a segmental colon resection by laparoscopy. The histological examination of the surgical specimen revealed a partially necrotic submucosal lipoma.
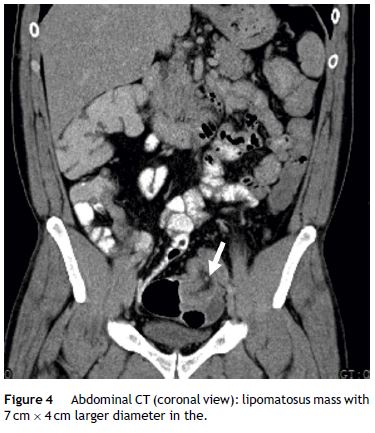
The authors describe this case due to its rarity. Colonic lipoma is a very rare benign tumor, however it is the second most common benign tumor of the colon with an incidence between 0.2 and 4%.1 In 90% of these cases the origin of the lipoma is confined to the submucosal layer.2 It is more frequently found in the right colon by colonoscopy. These lesions are usually asymptomatic and do not require specific treatment. Lipomas larger than 4 cm, are considered giant and are symptomatic in 75% of cases.3 Symptoms are usually abdominal pain, bleeding, colonic obstruction and intussusception. The intussusception is a rare complication that requires a differential diagnosis with a malignant lesion. Literature describes that lipomas larger than 2 cm should be removed due to colonic intussusception risk.4
The treatment for symptomatic lipomas has typically included surgical resection, but the use of minimally invasive techniques such as endoscopic therapy is increasing.4 Thus, various endoscopic procedures, including snare resection, endoscopic submucosal dissection, unroofing, endoloop technique and a combination of the last two, the “grasp-to-retract, ligate, unroof, and let-go” technique have been introduced recently for safe resection4.4,5 In this case, the patient underwent a surgical resection because he presented with an acute colonic obstruction from intussusception.
References
1. Vecchio R, Ferrara M, Mosca F, Ignoto A, Latteri F. Lipomas of the large bowel. Eur J Surg. 1996;162:915-9. [ Links ]
2. Michowitz M, Lazebnick N, Noy S, Lazebnik R. Lipoma of the colon. A report of 22 cases. Am Surg. 1985;51:449-54. [ Links ]
3. Huh KC, Lee TH, Kim SM, Im EH, Choi YW, Kim BK, et al. Intussuscepted sigmoid colonic lipoma mimicking carcinoma. Dig Dis Sci. 2006;51:791-5. [ Links ]
4. Lee JM, Kim JH, Kim M, Kim JH, Lee JB, Lee JH, et al. Endoscopic submucosal dissection of a large colonic lipoma: report of two cases. World J Gastroenterol. 2015;21:3127-31. [ Links ]
5. Ponte A, Pinho R, Vale S, Fernandes C, Ribeiro I, Silva J, et al. Resection of a large ileal lipoma exhibiting ball-valve prolapse into the cecum with a grasp-to-retract, ligate, unroof, and let-go technique. Endoscopy. 2015;47:E215-6. [ Links ]
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Authorship
Filipa Ávila did the writing of the manuscript. All authors were responsible for the revision of its contents.
Conflicts of interest
The authors have no conflicts of interest to declare.
* Corresponding author.
E-mail address: filipaavila@gmail.com (F. Ãvila).
Received 10 January, 2016; accepted 3 April 2016














