Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
GE-Portuguese Journal of Gastroenterology
versão impressa ISSN 2341-4545
GE Port J Gastroenterol vol.25 no.5 Lisboa out. 2018
https://doi.org/10.1159/000485804
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
Colonic Gallstone Ileus: A Rare Case
Ileus biliar cólico: um caso raro
Cristina Teixeira, Ana Luisa Alves, Isabelle Cremers
Gastroenterology Department, Centro Hospitalar de Setúbal, Setúbal, Portugal
* Corresponding author.
Keywords: Cholelithiasis, Colonic gallstone ileus
Palavras-Chave: Colelitíase, Íleus biliar cólico
Case Report
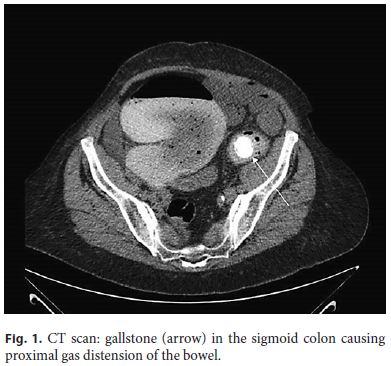
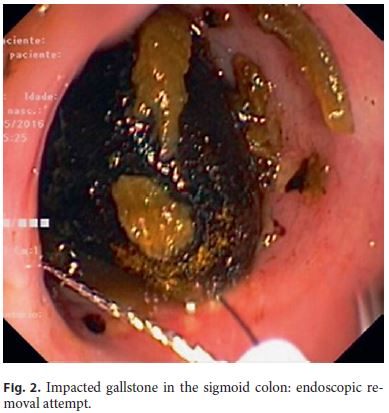
A 72-year-old woman with a history of atrial fibrillation, arterial hypertension, thyroidectomy, and mitral insufficiency presented to the emergency department with nausea, vomiting, and abdominal pain for the last 24 h. At physical examination, the patient had right upper abdominal pain and Murphys sign. Abdominal ultrasound revealed gallstones, thickened gallbladder wall, and sonographic Murphys sign. Blood tests showed normal liver tests and inflammatory parameters (INR 2.1). She was admitted for acute cholecystitis. Due to comorbidities, intravenous antibiotherapy was started and cholecystectomy was delayed until cardiac evaluation and anticoagulation correction. On the 6th day of hospitalization, the patient presented abdominal distension, hyperactive bowel sounds, and mild diffuse tenderness. CT scan demonstrated a thickened gallbladder wall with fistula to the colonic hepatic flexure, and a gallstone of 2.2 cm in the sigmoid colon causing proximal gas distension of the bowel (Fig. 1). Colonoscopy revealed an impacted gallstone at 30 cm from the anal verge and adjacent mucosal ulceration (2 ulcers of 5 mm). Attempted endoscopic removal with snare and basket was unsuccessful (Fig. 2). Due to colonic distension and higher surgical risk associated with the one-stage procedure, the patient underwent enterolithotomy and cholecystectomy was delayed and performed 2 months later, without complications.
Discussion
Gallstone ileus is responsible for 1–4% of cases of intestinal obstruction and occurs predominantly in females [1]. Biliary-enteric fistulas occur in the setting of inflammation, as acute cholecystitis and gallstones must be at least 2–2.5 cm in diameter to cause obstruction. The most common site of impaction is the terminal ileum and the ileocecal valve. Colonic gallstone ileus occurs in 4% of the cases, mostly at the level of the sigmoid colon [2]. Clinical presentation of gallstone ileus depends on the site of impaction and may include abdominal pain and distension, nausea, vomiting, and constipation. Diagnosis is difficult and in many cases, it is intraoperative. CT of the abdómen and pelvis remains the gold standard with sensitivity and specificity rates of 3 and 100%, respectively [1]. The classical radiological triad as described by Rigler et al. [3] includes pneumobilia, dilated small bowel, and aberrant gallstone location. Surgery is the mainstay of treatment. Methods of approach include: enterolithotomy alone (with or without a sequential cholecystectomy) or enterolithotomy, cholecystectomy, and fistula repair as a onestage procedure. The one-stage procedure is related to higher perioperative morbidities and mortality [4]. Endoscopic retrieval of the stone may be attempted but is rarely successful. Other approaches include extracorporeal or electrohydraulic lithotripsy [4].
References
1 Clavien P, Richon J, Burgan S, et al: Gallstone ileus. Br J Surg 1990;77:737–742. [ Links ]
2 Reisner R, Cohen J: Gallstone ileus: a review of 1,001 reported cases. Am Surg 1994;63:441–446. [ Links ]
3 Rigler L, Borman C, Noble J: Gallstone obstruction: pathogenesis and roentgen manifestations. JAMA 1941;117:1753–1759. [ Links ]
4 Nuño-Guzmán CM, Marín-Contreras M, Figueroa-Sánchez M, et al: Gallstone ileus, clinical presentation, diagnostic and treatment approach. World J Gastrointest Surg 2016;8:65–67. [ Links ]
Statement of Ethics
This study did not require informed consent nor review/approval by the appropriate ethics committee.
Disclosure Statement
All authors have read and approved the manuscript and deny conflicts of interest.
* Corresponding author.
Dr. Cristina Teixeira
Gastroenterology Department, Centro Hospitalar de Setúbal
Rua Camilo Castelo Branco
PT–2910-446 Setúbal (Portugal)
E-Mail ac.corda.teixeira@gmail.com
Received: September 22, 2017; Accepted after revision: November 28, 2017
Author Contributions
C.T., A.L.A., and I.C. were involved in the management of the case. The manuscript was prepared by C.T. and was vetted by all.














