An 83-year-old man with arterial hypertension and benign prostatic hyperplasia was referred for chronic intermittent watery diarrhea, colicky abdominal pain, asthenia, anorexia, and weight loss (15-20 kg, a 33% loss of body weight) with a year of evolution. He denied fever, skin changes, and arthralgia. The patient became dependent on others for daily routine activities. Periods of confusion and disorientation were also reported. On physical examination, evidence of severe cachexia (body mass index 15.7 kg/m2), a painless abdomen without ascites, and no palpable lymphadenopathy were observed. Upper gastrointestinal endoscopy showed duodenal diffuse whitish stippling, whose histopathological examination reported lymphangiectasias. Ileocolonoscopy with biopsies was unremarkable. Laboratory examinations revealed increased erythrocyte sedimentation rate (65 mm/h; normal: 1-20 mm/h), increased C-reactive protein (9.4 mg/dL; normal: <0.5 mg/dL), mild lymphopenia (0.9 × 109/L; normal: 1-3 × 109/L), hypochromic microcytic anemia (hemoglobin 7.8 g/L; normal: 13-17.5 g/L, mean corpuscular volume 69.9 fL; normal: 83-101 fL), elevated prothrombin time (15.5 s; control: 11.4 s), hyponatremia (130 mmol/L; normal: 136-146 mmol/L), and hypoalbuminemia (1.9 g/dL; normal: 3.5-5.2 g/dL). Stools examination for bacteria and parasites were negative. Fecal calprotectin was superior to 6,000 mg/kg (normal: <50 mg/kg). Interferon gamma release assay, human immunodeficiency virus, and chromogranin A were negative, and thyroid function was normal. Abdominopelvic computed tomography scan identified infracentimetric hypodense ileocolic lymph nodes. On suspicion of a protein-losing enteropathy, a Pillcam®SB3 capsule endoscopy (Given Imaging Ltd., Yoqneam, Israel) was performed revealing the entire mucosa of the small bowel diffusely edematous with prominent whitish spots (Fig. 1a-c). These endoscopic features led to the suspicion of Whipple disease. To confirm the diagnosis, the patient underwent upper gastrointestinal endoscopy in our institution with duodenal biopsies (Fig. 2). Histopathological examination revealed ectatic lymph vessels in lamina propria and multiple periodic acid-Schiff positive macrophages (Fig. 3a, b). Polymerase chain reaction testing for Tropheryma whipplei DNA was positive. The patient was admitted and started antibiotic treatment with ceftriaxone 2 g intravenous once daily for 2 weeks followed by trimethoprim-sulfamethoxazole 160/800 mg twice daily for 1 year. Additionally, parenteral nutrition, personalized diet, and physical rehabilitation were given on a multidisciplinary basis involving nutritionist and physiatrist. Response to treatment was dramatic with diarrhea resolving within several days, significant weight gain in few months and progressive regain of autonomy for daily activities. Reassessment laboratory examinations at 6 and 10 months revealed a normalization of hemoglobin (14 g/dL), serum sodium, albumin (4 g/dL), and C-reactive protein (0.5 mg/dL) levels.

Fig. 1: a-c - Capsule endoscopy showing the entire mucosa of the small bowel diffusely edematous with prominent whitish spots
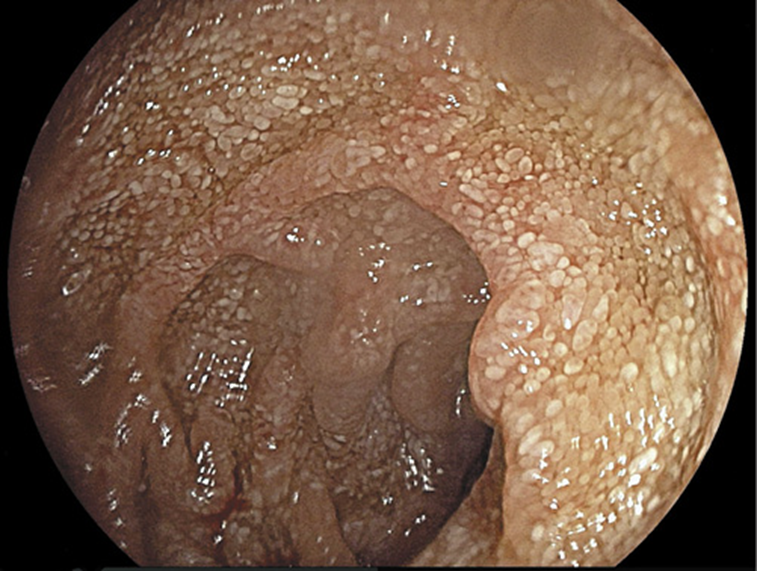
Fig. 2: Upper gastrointestinal endoscopy revealing whitish small plaques diffusely distributed in the intestinal mucosa of the second portion of the duodenum.
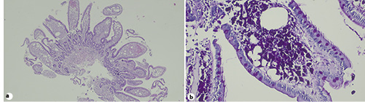
Fig. 3: a, b Histopathological examination of duodenal biopsies by upper gastrointestinal endoscopy showed ectatic lymph vessels in lamina propria and multiple periodic acid-Schiff-positive macrophages.
Whipple’s disease is a chronic and rare multisystemic infection caused by the Gram-positive bacillus Tropheryma whipplei, affecting predominantly white middle-aged males (1). Upper gastrointestinal endoscopy with biopsies of the small bowel is the diagnostic test of choice, but in some cases, may not establish the diagnosis. In this subset of patients, the capsule endoscopy can have a decisive diagnostic role, especially in a high suspicion of a diffuse but patchy enteropathy, even with nondiagnostic upper gastrointestinal endoscopy with biopsies and abdominal imaging. There are a few cases in the literature describing the almost pathognomonic capsule endoscopic finding of diffuse whitish stippling with or without villous atrophy, erosions, lymphatic ectasia, areas of denuded mucosa (2-5). We presented an atypical case of Whipple disease not only for the patient’s age but also for the endoscopic modality that was decisive in establishing the diagnosis.















