Introduction
The bifid condyle is a rare anatomic condition that was reported for the first time by Hrdlička in 1941 in a specimen skull.
This condition is manifested by a depression or deep cleft in the center of the condylar head with an anteroposterior or mediolateral orientation. Its etiology is not well known and may be somewhat diversified, as it may be associated with a congenital malformation, trauma, or even tumoral lesions.1,2
The bifid condyle is generally an accidental finding in routine radiographic exams. It may be detected first in a panoramic radiograph, and then, a computed tomographic exam may be performed as an alternative method of diagnosis.3 For the correct diagnosis of the bifid condyle, the two‑dimensional panoramic radiographic image alone would not be sufficient because it could lead the examiner to considering other anomalies such as condylar hyperplasia or osteochondroma. On the other hand, in 3D images obtained using cone‑beam computed tomography, these three conditions are shown differently.4
The association between the condylar heads’ orientation and the bifid condyle is controversial between authors. According to Dennison et al.,5 only an anteroposterior orientation of the condyle represents a “true” bifid condyle, while the mediolateral orientation would be a “condylar nothing.” On the other hand, Lopez‑Lopez6 defends that the condylar heads’ orientation is not an indicator of the bifid condyle and both condylar heads have to emerge from the condylar neck in order to be considered true bifid condyles.
After the diagnosis has been defined, the appropriate treatment for the case can be determined. In the absence of symptoms, adequate follow‑up must be maintained to improve the patient’s quality of life.7 In symptomatic cases, depending on their severity, different treatments must be performed according to the symptoms. Non‑steroid anti‑inflammatory drugs, analgesics, physical therapy, and occlusal plates are recommended as a conservative approach. Surgical treatment has been described only for restoring the function of a bifid condyle with ankylosis or symptomatic cases that have been resistant to conservative treatment.8
The present study aimed to report a case of a unilateral bifid condyle of unknown etiology in a patient who presented to the surgery clinic of the Department of Dentistry of the Pontifical Catholic University of Minas Gerais (PUC‑Minas) for third‑molar extraction. When imaging exams were requested, an uncommon anatomic shape was observed in the mandibular condyle on the left side.
Case report
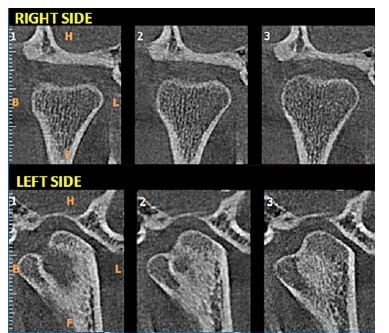
A 27‑year‑old male patient presented to the Department of Dentistry of PUC‑ Minas to evaluate the possibility of extracting his third molars. During anamnesis, the patient reported no systemic changes. Intraoral and extraoral examinations revealed no changes in the following aspects: facial symmetry without functional changes, lateral and protrusion movements without pain complaints, no deviations, and no compromising mouth opening and closing. Following the University’s protocol for third‑molar and supernumerary‑teeth evaluation in the region, a panoramic radiograph was requested. It revealed radiopaque images added to the condylar head on the left side, causing morphological changes.
These findings suggested the diagnostic hypothesis of a unilateral bifid condyle (Figure 1). A cone‑beam computed tomography scan was requested to obtain sufficient sagittal, axial, and coronal tomographic images for a 3D reconstruction. This reconstruction allowed better visualization of the condyle in the three spatial planes and its position in relation to the mandibular fossa (Figures 2, 3, and 4). The exam showed evidence of unilateral hyperdense masses on the left, in the shape of secondary mediolaterally oriented condylar heads. Although these were contiguous to the condylar head, a constriction between them was noted in the superior condylar pole region, as demonstrated by the 3D reconstruction and sagittal sections (Figure 3). Despite the morphological change noted in the left condyle, the anatomic structure was uniform, and the patient reported no functional change (Figure 4). Therefore, the diagnostic hypothesis of a left unilateral bifid condyle was confirmed.
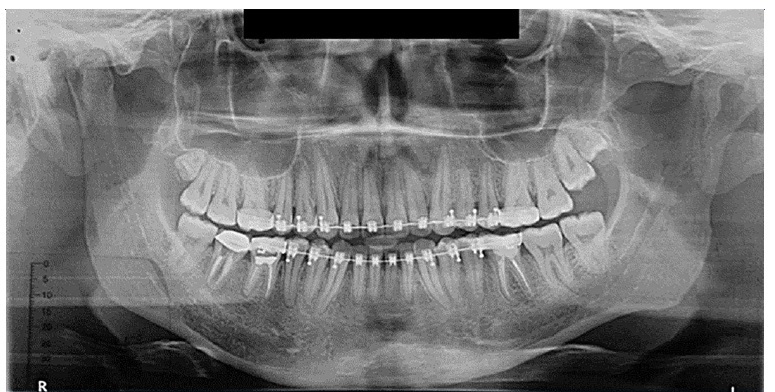
Figura 1 Panoramic radiograph showing an uncommon shape of the left mandibular condyle with radiopaque masses added to its superior portion
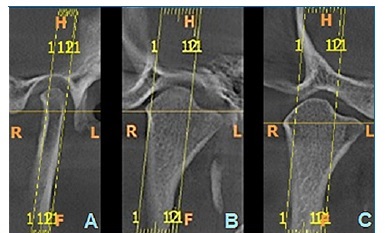
Figura 2 Tomographic sections of the left condylar process. A. Coronal Section - Closed Mouth; B. Sagittal Section - Closed Mouth; and C. Sagittal Section - Open Mouth
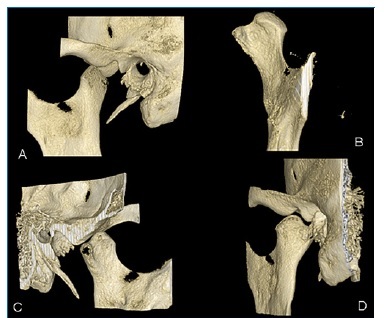
Figura 3 Three‑dimensional reconstruction of the condylar process. A-side view; B - anterior view; C - medial view; D - posterior view
On the right side, coronal reconstructions of the condylar process showed flattening on the superior pole. On the left side, the condylar process showed beveling of the superior pole, with a bifurcation and formation of two articular surfaces, thus exhibiting evidence of bifid condyle. In addition, a morphological adaptation of the mandibular fossa on both sides was noted, with flattening on the right side and sinuous ridges on the left side, accompanying the shape of the condylar processes (Figure 4).
As the condition was asymptomatic in this patient, no interventional treatment was performed at this time. However, active monitoring through imaging exams was recommended.
Moreover, the patient was recommended to seek professional care at the University clinic if any change occurred in his clinical condition. At present, the patient is being followed with clinical and radiographic exams, and annual follow‑ups are foreseen.
Discussion and conclusions
The condition of unilateral bifid condyle manifested by a secondary condylar head is a most uncommon finding. In the case presented, the clinical findings were in agreement with those reported in a retrospective study,9 in which 40% of the cases observed were asymptomatic and generally associated with a non‑traumatic etiology, frequently detected during a routine exam for the removal of third molars.
Concerning the prevalence between sex and age, according to a systematic review,8 patients with bifid condyle had an average age of 30.6 years, with women being more frequently affected than men in a ratio of 4:1. Unilateral impairment was the most prevalent condition, although there was a notable proportion of bilateral bifid condyle.8 In the present case, the 27‑year‑old patient was affected by a unilateral condition.
Bifid condyle’s etiology is not well known. It can be considerably diversified and may be associated with a congenital malformation, trauma, infection, nutritional disorders, radiation exposure, developmental abnormalities, teratogenic embryopathy, tumors, or condylectomy.10 In this case report, the patient did not report any trauma or surgery and did not present with symptoms and clinical signs that could indicate the causal factor.
Shriki et al.11hypothesized that the bifid condyle with a mediolateral orientation of the head was a developmental phenomenon and not the result of trauma. Accordingly, many studies have reported that most patients who had mediolateral bifid condyles had no history of trauma.12In the present case, this possibility was not considered, as the patient did not report any previous trauma.
The condyle’s morphology is a controversial topic regarding the factors that characterize a “true” and a “false” bifid condyle. According to Lopez‑Lopez,6 the orientation of these condylar heads is independent of the condition and a “true” bifid condyle depends only on both heads emerging from the condylar neck.6 In the present case, the condyle was located in the mediolateral direction, in agreement with the situation proposed by these authors. Therefore, the bifid condyle was in the axial and coronal projections of the mandible as bilateral hyperdense bony masses in the shape of secondary mediolaterally oriented condylar heads. Although they were apparently contiguous with the condylar head, a constriction was observed between the two parts.
Because the panoramic radiograph was not specific, for a complete visualization of the bifid condyle, a 3D tomographic reconstruction was produced in this study. The same was described by Tanner et al.3 On the other hand, Dennisson et al. [5] considered that the mandibular condyles were oriented obliquely, and therefore, the condylar heads could not be visualized in a single projection.3
The appropriate treatment for the bifid condyle depends on the symptoms presented. Some authors13 believe that this condition plays a role in some cases of temporomandibular disorder (TMD) and may be confused with an early diagnosis of condylar fracture; this shows the importance of a correct diagnosis. After careful clinical examination combined with complementary imaging exams, patients diagnosed with internal articular derangement should be treated according to the severity of the condition, which may include using occlusal splints and arthroscopic surgery.7 In asymptomatic cases, such as the one described in this case report, patients must be followed up and require no intervention if functional changes are not observed.
The bifid condyle can also be a differential diagnosis of pathologies such as condylar hyperplasia and osteochondroma.
However, knowledge of its clinical and imaging presentation is necessary. Moreover, before performing other complementary exams, differentiation between the above‑mentioned conditions is recommended through methods such as scintigraphy and histopathology. It is worth emphasizing that, for a correct diagnosis, a ideally, clear differentiation should be observed between the two pathological changes cited. Therefore, scintigraphy or even a histopathological exam must be performed to detect bone development at the site.4
Osteochondroma is pointed out as being one of the most common benign bone tumors that mainly affect the long bones. Intraorally, its highest prevalence is in the condyle and mandibular coronoid processes. It is frequently discovered through routine imaging exams, as the bifid condyle. The osteochondroma is usually treated with surgical excision in a procedure denominated low condylectomy.4 Conversely, in asymptomatic cases of bifid condyles, such as the one here reported, there is no need for intervention.
In turn, in condylar hyperplasia, a more regular contour is observed, showing an inverted pyramid with an increased volume of the mandibular head and a longer neck.14 The bifid condyle here presented was visualized as unilateral hyperdense masses in the shape of secondary mediolaterally oriented condylar heads. Although they were contiguous to the condylar head, a constriction between them was noted in the mandibular notch region (mandibular incisure).
The individual evaluation of panoramic radiographs leads to an incorrect diagnosis of bifid condyle cases because of this technique’s technical limitations, such as superimpositions and loss of some details, like any other bidimensional visualization.15 Therefore, tomographic images are pointed out as decisive for the final diagnosis of this condition. Furthermore, there is an increasing incidence of bifid condyle as more high‑quality exams become available, proving the need for studies on this condition.15 In the case described, a panoramic radiograph was initially requested, and then a cone‑beam computed tomography was performed as a complementary imaging exam to determine the diagnosis.
In conclusion, the dentists’ clinical experience must include knowledge of rare conditions such as the bifid condyle because this variation from normality is the differential diagnosis of pathological conditions such as condylar hyperplasia and osteochondroma. These three conditions have similar radiographic aspects and can lead the clinician to suspect a previous fracture of the condylar process, suggesting a potential change in the mandibular shape since this concerns an area related to growth. The possibility of causing functional changes in the patient, such as TMD, leads to the need for a more meticulous assessment of changes that may be associated with the case, such as limited or altered mandibular movements. Therefore, the professional must know how to distinguish these lesions and promote a correct diagnosis. For this to occur, the dentist must be aware of the indications when requesting complimentary exams to reach a diagnosis and elaborate a feasible treatment plan.