Introduction
The great majority of malignant cervical lesions is associated with human papilloma virus (HPV) positivity1,2. Nevertheless, 5,5-11% are reported as HPV-negative3. Additionally, false-negative cytology occurs in 27,1% of cases2. When presenting simultaneously, diagnostic delay may occur.
Hematometrocolpos corresponds to blood retention in the uterine cavity and cervix. When presenting in postmenopause, an underlying malignant cause should be investigated4.
Description of the case
A 74-year-old multiparous woman, with chronic hypertension and type 2 diabetes, had had previous excision of the transformation zone (TZ) due to high-grade squamous intraepithelial lesion (HSIL) at 39 years old. She was referred for specialist care at 70 years old following a cytologic HSIL. Colposcopy revealed TZ 3. A new excision of TZ showed cervical intraepithelial neoplasia (CIN) 3 with free margins. Follow-up until the third year was uneventful, with negative exams.
At the third year of follow-up, a flat cervix was observed. A negative co-test was obtained once more. A pelvic ultrasound was performed, discovering hidrometrocolpos (Figure 1), which was corroborated by computed tomography scan. For pain relief, the intracavitary content was drained by cervical permeabilization with a hysterometer and it was hematic.
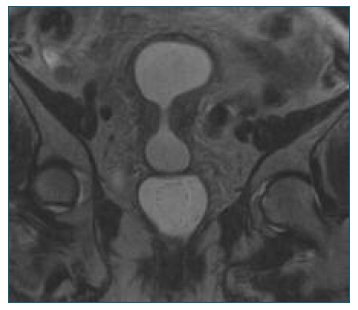
Following uterine bleeding and recidive of hematometrocolpos, a hysteroscopy was performed. A suspicious cervical mass was unveiled and biopsied. Despite an endometrial polypoid image was observed, poor visualization precluded its safe excision. Endocervical biopsies showed CIN 3 and could not unequivocally exclude stromal invasion. Magnetic resonance imaging (MRI) described a cervical neoplasm (Figure 2) and the patient was referred to an Oncology Reference Center.
Endocervical curettage identified HPV-16 and suggested low-grade squamous intraepithelial lesion. The hysteroscopic biopsies were revised in the Oncology Center. One fragment was concordant with squamous cell carcinoma in situ with involved margins. Another one showed stratified squamous epithelium with HSIL and colonization of endocervical glands, with features of stromal invasion.
The MRI was revised and an endometrial lesion with cervical extension was suggested. Positron emission tomography showed high-metabolism lesion involving the inferior third of the endometrium and the cervix. After multidisciplinary discussion, the tumor origin was considered unclear. MRI in the Oncology Center was performed, supporting a cervical origin. No other suspicious lesions were identified. A renal ultrasound was performed due to decreased renal clearance (diabetic and hypertensive-kidney disease), showing no hydronephrosis. Considering the presence of invasive carcinoma and greater dimension of tumor of 4 cm, stage IB2 from 2018 FIGO classification for cervical cancer was assumed.
Considering advanced age and comorbidities impeding surgery and low renal clearance hindering chemotherapy, isolated radiotherapy was decided. The patient was submitted to intensity-modulated radiation therapy (45Gy/25 fractions) followed by high-dose-rate intrauterine brachytherapy (24Gy/3 fractions). She presents no clinical nor imagiologic signs of recidive at one-year follow-up.
Conclusions
The clinical presentation of cervical cancer may be atypical, with negative co-test and presentation of hematometrocolpos. Advanced age and inherent limitations of HPV tests may contribute to its false-negative results3. Differential diagnosis with endometrial neoplasia may be difficult. A low threshold of suspicion should be kept when facing hematometrocolpos in a postmenopausal woman4.
Author’s contribution
Marta Gomes de Melo was responsible for the conceptualization, clinical care of the patient - diagnosis, and writing - original draft, review and editing. Rita Marquez Passarinho was responsible for clinical care of the patient - diagnosis, and writing - review and editing. Andreia Relva was responsible for clinical care of the patient including diagnosis, treatment and follow-up and writing - review and editing.