Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Similars in
SciELO
Similars in
SciELO
Share
Angiologia e Cirurgia Vascular
Print version ISSN 1646-706X
Angiol Cir Vasc vol.12 no.3 Lisboa Sept. 2016
https://doi.org/10.1016/j.ancv.2016.04.002
CASE REPORT
Post-traumatic femoropopliteal pseudo-aneurysm in a patient allergic to heparins
Pseudoaneurisma femoropoplíteo pós-traumático em doente alérgico às heparinas
Carla Lorena Blanco Amil*, Carolina Gallego Ferreiroa, Eduardo Fraga Munoz, José Manuel Encisa de Sá
*Vascular and Endovascular Surgery Department, Hospital Álvaro Cunqueiro, Vigo, Spain
ABSTRACT
Post-traumatic pseudo-aneurysms of the femoral artery are a rare complication.
They normally have iatrogenic causes and immediately appear. Less often, they appear at a later stage and are related with traumatisms, orthopaedic surgery, bone lesions, infections, etc.
This report presents a case of a patient with allergy to heparin, and pseudo-aneurysm of the superficial femoral artery and 1st portion of the popliteal artery secondary to remote trauma in an extremity with serious deformities as a sequel. We performed conventional surgery using a posterior approach, and obtained a satisfactory outcome and evolution.
Keywords: Femoropopliteal pseudo-aneurysm; Post-traumatic pseudoaneurysm; Posterior approach; Heparin allergy
RESUMO
Os pseudoaneurismas pós-traumáticos da artéria femoral são uma complicac¸ão rara. Normalmente têm causa iatrogénica e aparecem de imediato. Menos frequentemente surgem numa fase tardia e costumam estar relacionados com traumatismos, cirurgia ortopédica, lesões ósseas, infeções, etc.
Este artigo apresenta o caso de um paciente alérgico àheparina com pseudoaneurisma da artéria femoral superficial e primeira parte da artéria poplítea, secundário ao traumatismo remoto de uma extremidade com sérias deformidades como sequela. Realizamos cirurgia convencional com abordagem posterior e obtivemos um resultado e evoluc¸ão satisfatórios.
Palavras-chave: Pseudoaneurisma femoropoplíteo; Pseudoaneurisma pós-traumático; Abordagem posterior; Alergia à heparina
Introduction
Post-traumatic pseudo-aneurysms of the femoral artery (FA) are a rare complication. The most common etiologies are iatrogenic punctures.1 Nevertheless, there are cases that arise gradually causing pseudo-aneurysms at a later time. In these cases we should perform a differential diagnosis for other possible causes.2--10 The most common clinical expression appears immediately in the context of percutaneous procedures. They appear as pulsatile masses with ecchymosis near the puncture. This is accompanied by symptoms arising from compressing adjacent structures. When they appear later in time, they are generally asymptomatic. They are diagnosed incidentally or due to complications appearing from local compression, distal embolization, thrombosis or rupture. The therapeutic approach is similar to that used for atherosclerotic aneurysms at this level. Even though open surgery remains the treatment of choice, endovascular repair is becoming increasingly used due to its low morbidity and mortality and good patency.
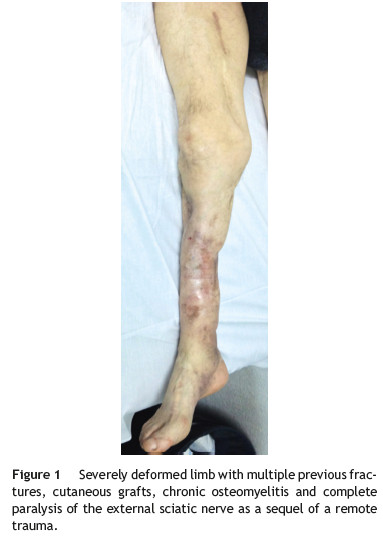
We report a case of a patient that presented a femoropopliteal pseudo-aneurysm in a severely deformed limb with multiple cutaneous grafts, chronic osteomyelitis and complete paralysis of the external sciatic nerve as a sequel of a remote trauma. In addition he presented allergy to heparin, detail that made change our therapeutic attitude.
Case report
We present the case of a 53-year-old male with a previous history of allergy to neomycin, hypertension, and dyslipidemia. The patient had quit smoking 4 years earlier. The patient had suffered a traffic accident 25 years before causing a supracondylar fracture of the right femur, open fracture of the tibia and fibula with secondary acute ischaemia. The patient needed stabilization of the tibia and fibula with a Hoffmann external fixator and osteosynthesis of the fracture using Kirschner needles. Another health centre performed this. The arterial reconstruction was unknown and needed multiple skin grafts to cover it. As a sequel, the patient suffered complete paralysis of the external sciatic nerve and chronic osteomyelitis of the tibia.
The patient was admitted to our service for a pulsatile lump, located on the inner face of the right thigh. This had appeared 18 months earlier and had increased in size. The clinical picture was accompanied by occasional discomfort in the limb and at the level of the lump; but without affecting the quality of ambulation. On physical examination we palpated a pulsatile lump on the inner face of the right thigh. This lump was about 7 cm in length. The patient presented coldness in his foot, with slowed venous-capillary refilling, and on vascular exploration, he presented a femoral pulse, but absence of popliteal and distal pulses. The severe deformity of the limb after trauma with multiple cutaneous grafts is highlighted (Fig. 1).
The computed tomography angiography (CTA) revealed a roughly 76 mm diameter pseudo-aneurysm of the distal superficial femoral artery (SFA), with mural thrombus and internal calcifications. The popliteal artery was difficult to see due to bone fixation material artefacts. The tibioperoneal trunk (TPT) was permeable with a peroneal artery as the only distal vessel. The anterior and posterior tibial arteries were occluded from the beginning (Fig. 2A, B).

Among the various therapeutic options, we initially chose placing a Viabahn® endoprosthesis since it is the less aggressive choice in a greatly deformed extremity (fractures, previous surgery, grafts, etc.). However, 4 days after admission, the patient suffered an allergic reaction to low molecular weight heparin (LMWH). We performed allergy tests (prick tests and intra-dermoreaction), which proved negative in the immediate reading and positive at 48 h for sodium heparin, enoxaparin, Fraxiparine, and bemiparin and negative for Fondaparinux. We diagnosed the patient for delayed hypersensitivity reaction to sodium heparin and LMWH except for Fondaparinux.
Due to this diagnosed allergy, we discarded Viabahn® endoprosthesis placement, since this contains a heparin coating, and opted for surgical treatment. We decided to carry out a diagnostic arteriography (Fig. 2C, D) in which we observed pseudo-aneurysm of the SFA and 1st portion of the popliteal artery, occlusion of the 2nd portion, and repermeabilisation of the 3rd portion. The TPT was permeable with outflow from the peroneal artery as the only exit vessel.
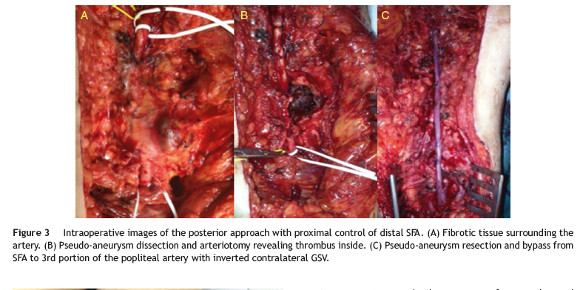
Considering the serious limb deformity and previous surgeries, we decided to use a posterior approach to the popliteal artery. We performed the pseudo-aneurysm resection and a bypass from the SFA to the 3rd portion of the popliteal artery with the inverted contralateral great saphenous vein (GSV) (Fig. 3A-C). During the procedure, we did not use systemic or local heparinisation, and only used an intraoperative plasma volume expander infusion (Voluven® 6% hydroxyethyl starch 130/0.4 in 0.9% sodium chloride).
The patient showed good postoperative evolution. Immediate complications included revascularization oedema that progressively remitted. The patient was discharged from hospital after 10 days, with a permeable bypass and good distal perfusion with conserved motility and sensitivity. After 30 months of follow-up, the patient remains asymptomatic and with a permeable bypass (Fig. 4).

Discussion
Femoral pseudo-aneurysms are a rare injury. They mostly occur from iatrogenic causes after performing percutaneous techniques of arterial catheterization. This is related to the increased use of these techniques.1 However, in late-appearing pseudo-aneurysms, we must perform a differential diagnosis for other possible causes such as previous injuries, orthopaedic surgery or others,2,4 bone lesions,3,6 infections (Salmonella, Escherichia coli, Staphylococcus aureus),5,7 diseases of the connective tissue (Ehlers-Danlos syndrome, Marfan Syndrome),8,9 inflammatory arteritis,10 etc.
Given the low incidence, both treatment and diagnostic strategy are based on clinical series which include atherosclerotic aneurysms at the femoropopliteal level.
Different imaging techniques are useful for diagnosis, such as Doppler ultrasound, computed tomography angiography (CTA), magnetic resonance angiography (MRA) and angiography.
Conventional surgery is the technique of choice, but endovascular techniques are becoming increasingly used as they are less aggressive and have good medium term results.11,12
Endovascular treatment has advantages such as a low mortality (0.6-3.5%), a success rate of 97% and a short hospital stay. Piazza et al. recently published long-term outcomes of endovascular exclusion of popliteal aneurysms.13 Retrospective revision finds 46 endovascular repairs of which 93% of the cases were elective and the rest due to rupture or acute thrombosis. The primary patencies at 1, 3 and 5 years were 82%, 79% and 76% respectively, while the secondary patencies were 90%, 85% and 82% respectively.
It does not need general or local anaesthesia; thus reducing cardiac risk, and may be performed percutaneously or with a minimal incision.14 It must, however, meet selection criteria, such as having proximal and distal anchoring areas of at least of 2 cm, patency of at least one exiting blood vessel, avoid excessive tortuosity and avoid excessively long lengths of aneurysms. A >20 cm segment coverage turns out to be a negative predictor of permeability (p < 0.032) and could explain the greater failure of the stent.13 The longer the device, the greater the rigidity it exerts on the area distal to the landing zone. This is a probable cause of kinking or friction on the arterial wall over time.12,13 It is not recommended in patients who frequently flex their knees >90◦ due to working conditions (risk of fracture or thrombosis) or in patients with dual antiplatelet therapy contraindications.15 Also it is not recommended in young patients, good operative risk, one vessel run-off or popliteal occlusion. Surgical decompression may be necessary after time despite the aneurysm has been satisfactorily excluded. It is, therefore, a factor to consider when assessing open surgery versus endovascular treatment of long or ruptured aneurysms.13
In our case, because of multiple previous surgeries of the extremity, we decided to perform endovascular treatment by placing an endoprosthesis (Viabahn®) as this was the less aggressive choice. However, as this device is covered in heparin, we discarded this option after discovering heparin allergy. The patient presented a local skin reaction and delayed-type hypersensitivity which is the most frequently kind of reaction reported. Therefore Fondaparinux, a factor Xa inhibitor, was used instead of heparin. It is a safe alternative for heparin allergic patients due to its low allergic potential and lack of cross-reaction to heparins.
Surgical treatment is the classic technique of choice. It is indicated in patients with acceptable risk, with complex anatomy, symptoms or in the presence of more advanced degrees of acute ischemia.16 It presents an excellent primary patency at 1 year in 95.9% of cases,12,16-20 with a significantly lower rate of adverse events (greater amputation or reoperation) after 1 year.17 This suggests that it should be proposed as the first choice in all asymptomatic patients that are not otherwise contraindicated for surgery. The most frequently used surgical approach is the medial since it allows us to exclude larger aneurysms that need a more distal bypass allowing easy access to the GSV in its entire course. The main drawback is in aneurysms that affect the popliteal artery, as it does not allow their decompression after ligation. Numerous studies21 show that despite the proximal and distal ligature, in 30% of cases the aneurysm does not undergo thrombosis and continues to grow owing to the persistence of collateral patency. This causes pain, compression symptoms and rupture requiring reoperation. Some authors recommend the ligation of back-bleeding side branches, except in small aneurysms.15 This can usually be done from the supracondylar and infracondylar spaces.
The posterior approach is preferred for aneurysms confined to the popliteal space and represents the best choice to decompress aneurysms that have continued to grow after being treated as a result of the flow through genicular arteries. As a drawback it has more risk of nerve injury and is not recommended in cases of aneurysms that extend very proximally or distally.15
Here, in the case of a traumatic limb with numerous previous surgeries and skin grafts, the medial approach was inaccessible given the prior trauma. Thus, redissection would involve risk of nerve or muscle injury. Finally, we opted for the posterior approach since it represented a virgin approach, which, with a wide dissection, allowed us to deal with the aneurysm located in the distal SFA, and perform the distal anastomoses in the TPT.
Another challenging issue of this case was the necessity of Voluven® instead of heparin during vascular clamping reconstruction due to the heparin allergy diagnosed while his admission. Hydroxyethyl starches (HES) are synthetic colloids commonly used for fluid resuscitation to replace intravascular volume. First-generation HES have been reported to consistently decrease plasma concentrations of coagulation factor VIII and von Willebrand factor.22-23 HES also impair platelet function, likely via an extracellular coating mechanism.24 Several clinical trials have examined the effect of preoperative administration of third-generation HES on coagulation parameters after cardiac surgery and compared with other colloids.25 Schramko et al.26 assessed the effects of a short-term postoperative infusion of HES or human albumin on blood coagulation in primary elective cardiac surgical patients. Blood loss and transfusion requirements were similar in all groups. However, when compared with the albumin group, transient prolongation of clot formation times and decrease in clot firmness were observed in HES group.
Conclusions
Post-traumatic pseudo-aneurysms are a rare complication following trauma of extremities. Sometimes they are associated with serious deformities, which limit the surgical approach. Currently, the development of endovascular techniques allows us to treat them with a minimally aggressive approach, and with rates of patency approaching those of open surgery in selected patients (with favourable anatomy, high-surgical risk). However, it is not always applicable. Open surgery continues to be the treatment of choice, and the knowledge of both types of approach allows the treatment of complex cases.
References
1. Stone PA, Campbell JE, AbuRahma AF. Femoral pseudoaneurysms after percutaneous access. J Vasc Surg. 2014;60:1359-66. [ Links ]
2. Raherinantenaina F, Rajaonanahary TM, Rakoto Ratsimba HN. Femoral artery pseudoaneurysms encountered in orthopedics and traumatology. J Mal Vasc. 2015, http://dx.doi.org/10.1016/j.jmv.2015.08.001. [ Links ]
3. Regus S, Lang W. Arterial injury and pseudoaneurysm formation after lesser trochanter fracture. Int J Surg Case Rep. 2015;14:4-6. [ Links ]
4. Aldemir M, Adali F, Akci Ö, et al. A rare para-anastomotic femoral artery aneurysm in a patient with history of femoro-popliteal bypass graft occlusion. Int J Surg Case Rep. 2015;10:49-51. [ Links ]
5. Mahfood Haddad T, Vallabhajosyula S, Sundaragiri PR, et al. Mycotic pseudoaneurysm by vancomycin-intermediate Staphylococcus aureus: a rare cause of persistent bacteraemia. BMJ Case Rep. 2015, http://dx.doi.org/10.1136/bcr-2014209003. [ Links ]
6. Papacharalampous G, Galyfos G, Geropapas G, et al. False arterial aneurysm due to long bone exostosis: presentation of two cases and update on proper management. Ann Vasc Surg. 2015;29, 842.e19-22. [ Links ]
7. Karkos CD, Kalogirou TE, Giagtzidis IT, et al. Ruptured mycotic common femoral artery pseudoaneurysm: fatal pulmonary embolism after emergency stent-grafting in a drug abuser. Tex Heart Inst J. 2014;41:634-7. [ Links ]
8. Azghari A, Bouayad M, Belmir H, et al. Vascular type of Ehlers-Danlos syndrome: a rare cause of spontaneous pseudo-aneurysms. J Mal Vasc. 2010;35:254-8. [ Links ]
9. Baril DT, Carroccio A, Palchik E, et al. Endovascular treatment of complicated aortic aneurysms in patients with underlying arteriopathies. Ann Vasc Surg. 2006;20:464-71. [ Links ]
10. Ko GY, Byun JY, Choi BG, et al. The vascular manifestations of Behc¸et disease: angiographic and CT findings. Br J Radiol. 2000;73:1270-4. [ Links ]
11. Rancic Z, Pecoraro F, Pfammatter T, et al. Less invasive (common) femoral artery aneurysm repair using endografts and limited dissection. EJVES. 2013;45:481-7. [ Links ]
12. Midy D, Berard X, Ferdani M, et al. A retrospective multicenter study of endovascular treatment of popliteal artery aneurysm. J Vasc Surg. 2010;51:850-6. [ Links ]
13. Piazza M, Menegolo M, Ferrari A, et al. Long-term outcomes and sac volume shrinkage after endovascular popliteal artery aneurysm repair. EJVS. 2014;48:161-8. [ Links ]
14. Silistreli E, Karabay Ö, Erdal C, et al. Behc¸et's disease: treatment of popliteal pseudoaneurysm by an endovascular stent graft implantation. Ann Vasc Surg. 2004;18: 118-20. [ Links ]
15. Jacobowitz G, Cayne NS. Lower extremity aneurysms. In: Cronenwett JL, Johnston KW, editors. Rutherford's vascular surgery. 8th ed. China: Saunders; 2014. p. 2190-205. [ Links ]
16. Eslami MH, Rybin D, Doros G, et al. Open repair of asymptomatic popliteal artery aneurysm is associated with better outcomes than endovascular repair. J Vasc Surg. 2015;61: 663-9. [ Links ]
17. Pulli R, Dorigo W, Castelli P, et al. A multicentric experience with open surgical repair and endovascular exclusion of popliteal artery aneurysms. EJVS. 2013;45: 357-63. [ Links ]
18. Huang Y, Gloviczki P, Oderich GS, et al. Outcomes of endovascular and contemporary open surgical repairs of popliteal artery aneurysm. J Vasc Surg. 2014;60, 631-8.e2. [ Links ]
19. Dorweiler B, Gemechu A, Doemland M, et al. Durability of open popliteal artery aneurysm repair. J Vasc Surg. 2014;60: 951-7. [ Links ]
20. Cina CS. Endovascular repair of popliteal aneurysms. J Vasc Surg. 2010;51:1056-60. [ Links ]
21. Ravn H, Wanhainen A, Björck M. Surgical technique and longterm results after popliteal artery aneurysm repair. Results from 717 operated legs. J Vasc Surg. 2007;46: 236-43. [ Links ]
22. Claes Y, van Hemelrijck J, van Gerven M, et al. Influence of hydroxyethyl starch on coagulation in patients during the perioperative period. Anesth Analg. 1992;75:24-30. [ Links ]
23. Conroy JM, Fishman RL, Reeves ST, et al. The effects of desmopressin and 6% hydroxyethyl starch on factor VIIIC. Anesth Analg. 1996;83:804-7. [ Links ]
24. Wilkes MM, Navickis RJ, Sibbald WJ. Albumin versus hydroxyethyl starch in cardiopulmonary bypass surgery: a meta-analysis of postoperative bleeding. Ann Thorac Surg. 2001;72:527-33. [ Links ]
25. Haisch G, Boldt J, Krebs C, et al. Influence of a new hydroxyethylstarch preparation (HES 130/0.4) on coagulation in cardiac surgical patients. J Cardiothorac Vasc Anesth. 2001;15:316-21. [ Links ]
26. Schramko AA, Suojaranta-Yinen RT, Kuitunen AH, et al. Rapidly degradable hydroxyethyl starch solutions impair blood coagulation after cardiac surgery: a prospective randomized trial. Anesth Analg. 2009;108:30-6. [ Links ]
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
Conflicts of interest
The authors have no conflicts of interest to declare.
E-mail address: karlal48@hotmail.com (C.L. Blanco Amil).
Received 18 December 2015;
Accepted 13 April 2016
Available online 1 June 2016














