Introduction
The Eagle syndrome was first described by W. Eagle in 1937 who estimated the length of a normal styloid process at 2.5-3.0 cm.1 Two groups have been defined with elongated styloid (or calcified stylohyoid ligament), the classic form group and the vascular form group. The classic form is typically seen in patients after pharyngeal surgery. Ipsilateral cervical pain, dysphagia, sensation of a foreign body in the throat, tinnitus, or otalgia are all possible symptoms due to the anatomical proximity of cranial nerves V, VII, IX, or X. The vascular form, a rare presentation of this syndrome, is caused by the conflict with the vascular structures leading sometimes to carotid artery compression or even dissection and consequently aphasia, visual symptoms and limb motor and sensory deficit can be present. In addition, the simple stimulation of the artery sympathetic nerve plexus can cause pain along the artery course, as also eye pain and parietal headache. Being headache the most common initial symptom in patients with spontaneous dissection of the internal carotid artery,2 Eagle syndrome could be one explanation for some so-called spontaneous dissections, since the estimated incidence shows that 4% of population has an elongated process3,4 and, even though it is a rare condition, it may be under-reported. Despite this considerable incidence on general population, only a minority (4%) of these individuals present with symptoms, both in classical and vascular forms.
The aim of this review is to summarize the current evidence on the incidence and clinical implications of the vascular form of the Eagle syndrome. Fig 1.
Methods
We performed an electronic search of the literature using PubMed and Embase databases. The combination of key words used in our search strategy were the following: (Eagle syndrome OR stylocarotid syndrome) AND (carotid artery dissection OR compression OR stenosis). Only original publications in English and French were considered. Publications with insufficient information regarding patient characteristics, symptoms and treatment strategies were excluded.
Data on patient characteristics, presenting symptoms and treatment strategies were the extracted to compose our case study. For analysis, cases were included in one of two groups: internal carotid compression only and carotid dissection associated with elongated styloid process.
Results
After removing duplicated articles and fully reading the remaining articles, our focus was stablished in 44 case studies. After eliminating four cases with insufficient information, 40 cases reported in 33 publications were left.5,19,29,30,32,33,34,35,36-38 From these, 8 cases related to carotid artery compression and 32 cases of carotid artery dissection (CAD).
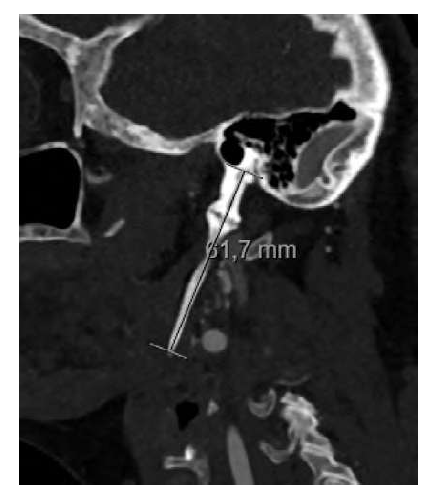
The carotid artery compression group consisted of 1 female and 7 male patients, with a mean age of 55.8 years. All cases presented with symptoms of hemihypoesthesia and/or weakness of one side of the body. Aphasia was reported in three cases and reduced field of vision in one. These transient neurological events were reported to be triggered by cervical rotation to the contralateral side of the affected body in five patients and regressive in neutral position. Just one patient had a history of right hemiparesis and aphasia resulting in long-term residual sequelae. Three case reports did not mention the cervical rotation as a factor, but multiple transient episodes were present in the clinical history. Six out of eight cases had clinical symptoms for over one year or more and only two patients presented with symptoms for less than a month. In terms of diagnostic imaging, dynamic computed tomographic angiography was the exam of election, which clearly showed an extrinsic compression of internal carotid artery in seven cases on the left side and in one on the right. Four patients had bilateral elongated styloid process and all patients were treated with surgical resection of the excessively long styloid process on the symptomatic side, except for one patient with bilateral involvement, who had a preventive resection. No patient had symptoms relapse after surgical management. Neither stenosis characterization nor medical treatment after surgical treatment were reported. Fig 2.
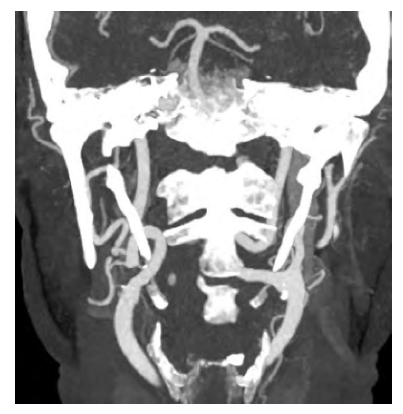
Figure 2 CT image showing the intimate relation between the internal carotid artery and the elongated styloid process leading to artery compression.
Among the 32 cases of CAD reported in the literature, 72% (23/32) were generally fit without reported comorbidities. The mean age of the group was 47.5 years old and 81% of the sample was in the interval of 40 to 60 years old. The condition was more common in men with a ratio of 2.2:1. Only 4 patients showed no focal neurological deficits and presented with sudden headache, being this symptom present in one third of the patients. Horner’s syndrome was reported in three. Computed tomography and/or magnetic resonance imaging (MRI) was performed and revealed bilateral styloid elongation in 19 of 32 patients and bilateral CAD in eleven. It also showed ischemic infarcts in 59% patients and dissecting aneurysms in five. Table 1.
Table 1 Synthesis of the 32 cases of CAD: demographic characteristics, clinical presentation and management;
| Cases | Sex | Age | Clinical Presentation | Initial management | Acute recurrence | Bilateral dissection | Ischemic infarcts on CT/MRI | Styloidectomy |
| AlAbdulwahed et al(5) | M | 35 | Focal neurological deficits | Antiaggregation | Yes | No | Present | Yes |
| Zuber et al(6) | F | 41 | Focal neurological deficits | Anticoagulation | No | No | Not present | No |
| Soo-O-yan et al(7) | F | 41 | Focal neurological deficits | Anticoagulation | No | No | Not present | No |
| Faivre et al(8) | M | 60 | Focal neurological deficits | Fibrinolysis | No | Yes | Present | Yes |
| Razak et al(9) | M | 41 | Focal neurological deficits | Fibrinolysis | No | No | Not present | Yes |
| Todo et al(10) | M | 57 | Focal neurological deficits | Anticoagulation | Yes | Yes | Present | No |
| Ogura et al(11)(1) | M | 55 | Focal neurological deficits | Anticoagulation nticoagulation | Yes | Yes | Present | Yes |
| Ogura et al(11)(2) | M | 55 | Focal neurological deficits | Stent placement | Yes | No | Present | No |
| Sveinsson et al(12)(1) | M | 38 | Focal neurological deficits | Fibrinolysis | Yes | No | Present | Yes |
| Sveinsson et al(12)(2) | F | 41 | Headache | Anticoagulation | Yes | No | Not Present | No |
| Yammamoto et al(13) | M | 51 | Horner Syndrome | Antiaggregation | No | No | Not present | No |
| Ohara et al(14) | M | 43 | Focal neurological deficits | Antiaggregation | No | No | Not present | No |
| Jo et al(15) | F | 38 | Headache | Antiaggregation | No | No | Not present | Yes |
| Subedi et al(16) | M | 57 | Focal neurological deficits | Stent placement | No | No | Present | Awaiting |
| Heban et al(17) | M | 57 | Focal neurological deficits | Antiaggregation | No | No | Present | No |
| Smoot et al(18) | M | 60 | Focal neurological deficits | Anticoagulation | Yes | No | Present | No |
| Zammit et al(20) | F | 45 | Horner syndrome | Antiaggregation | Yes | Yes | Present | No |
| Torikoshi et al(21) | M | 46 | Focal neurological deficits | Antiaggregation | Yes | Yes | Present | Yes |
| Galletta et al(22) | M | 53 | Focal neurological deficits | Fibrinolysis | No | Yes | Present | Yes |
| Baldino et al(23) | F | 41 | Headache | Stent Placement | No | No | Not Present | No |
| Baldino et al(23) | M | 48 | Focal neurological deficits | Anticoagulation | No | No | Present | Yes |
| Baldino et al(23) | M | 45 | Focal neurological deficits | Anticoagulation | No | Yes | Not Present | Yes |
| Baldino et al(23) | M | 49 | Focal neurological deficits | Anticoagulation | No | Yes | Not Present | Yes |
| Baldino et al(23) | M | 56 | Headache | Anticoagulation | No | No | Not Present | Yes |
| Takagi et al(24) | M | 30 | Focal neurological deficits | Antiaggregation | Yes | Yes | Present | No |
| Duarte-Celada et al(25) | F | 43 | Horner Syndrome | Stent Placement | No | Yes | Not Present | Yes |
| Horio et al(26) | F | 46 | Focal neurological deficits | Stent Placement | No | Yes | Present | Yes |
| Brassart et al(27) | F | 53 | Focal neurological deficits | Antiaggregation | Yes | No | Present | Yes |
| Mattioli et al(27) | M | 56 | Focal neurological deficits | Anticoagulation | No | No | Not present | No |
| Xhaxho et al(28) | M | 64 | Focal neurological deficits | Antiaggregation | No | No | Present | No |
| Selvadurai et al(31) | M | 17 | Focal neurological deficits | Fibrinolysis | Yes | No | Present | Yes |
| Aydin et al(37) | F | 57 | Focal neurological deficits | Antiaggregation | No | No | Present | No |
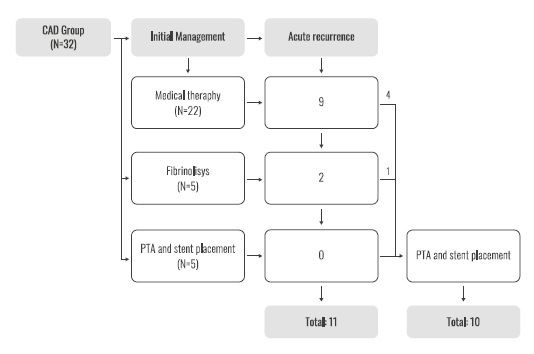
In terms of initial management, 22 patients were managed with medical therapy only: 11 with antiaggregating therapy and 11 with anticoagulation therapy, five underwent endovascular and/or intra-arterial fibrinolysis and five patients were managed initially with angioplasty and stent placement. Acute recurrence of symptoms was observed in 34% (11/32) of patients. Symptom recurrence was seen in nine patients who initially were treated with only medical therapy leading to balloon angioplasty and stent placement in four cases. Two of the five patients who underwent endovascular thrombectomy and/or intra-arterial fibrinolysis had also recurrence leading to stent placement in one. Overall, angioplasty with stent placement was done in a total of 10 patients and no acute recurrence symptoms were reported. After initial management seventeen patients were selected for styloidectomy on a semi-elective basis. Mean follow-up was 15.4 months and three cases reported recurrence symptoms during follow-up: two cases after stent placement awaiting styloidectomy and one case under medical therapy not selected for this procedure. Fig 3.
Discussion
Stylocarotid syndrome can vary in its clinical presentation. On one hand, in the compression group, patients present with reproducible symptoms with cervical rotation. Neurological sequelae are not common since these events are most transient. After establishing the relationship between the carotid artery and the styloid process, the treatment with surgical resection seems logical and very effective. To establish this relation dynamic imaging plays an important role. On the other hand, in CAD group, clinical presentation is usually sudden, and the best treatment is still unknown.
As for CAD, in the general population, there is lack of level I evidence regarding the best treatment and no consensus exists whether either antiaggregating or anticoagulation is more effective39,40 41,42. In our review there was no significant difference between the antiaggregating and anticoagulation therapy in terms of symptoms recurrence. Regardless, the recurrence rate is quite high in this group, since more than one third of patients experienced symptoms despite medical treatment. Moreover, the presence of the elongated process can explain why patients keep experiencing symptoms, possibly due to the progression of the dissection and distal embolization explained by the continuous impingement of the styloid process into the carotid artery.
Surgical or endovascular intervention is usually reserved for patients with deteriorating clinical neurologic symptoms despite medical treatment, compromised cerebral blood flow, contraindications to antithrombotic therapy, symptomatic or expanding aneurysm, high grade stenosis after 6 months or new or persistent aneurysm greater than twice the diameter of the normal internal carotid segment.2 A recent systematic review revealed the safety and technical feasibility of stenting in CAD,(40) making it likely that this procedure could be the treatment of choice, if the patient meets the criteria described above and, given that deteriorating clinical neurological symptoms are common in this subgroup of CAD. But, in this case it is mandatory to consider styloidectomy to prevent compression and/or fracture of the stent, unless the presence of a post dissection thrombosed aneurysmal sac is present keeping the stent away from the styloid process. Whether delayed styloidectomy after medical management plays a role in CAD, as it does for the compression group, remains undetermined.
Conclusion
Vascular Eagle syndrome should be considered part of differential diagnosis when confronting a young patient presenting either with transient neurological symptoms provoked by neck rotation or caused by CAD. Dynamic imaging is an important component in this setting as it can provide relevant information on surrounding relationship of the vascular structures. Although it is rare identity there is a growing number of case reports making it a possible explanation for some spontaneous CAD. Given the rarity of the condition, the ideal treatment has not yet been identified. Options include intra-arterial thrombolysis, surgical or endovascular repair, anticoagulation, and antiplatelet medication. Endovascular and surgical repair are considered a last resort but should be considered when dealing with a patient with recurrent dissection or lack of resolution. Resection of styloid process should also be contemplated on the management of carotid artery compression with or without CAD.