Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Similares en
SciELO
Similares en
SciELO
Compartir
GE-Portuguese Journal of Gastroenterology
versión impresa ISSN 2341-4545
GE Port J Gastroenterol vol.26 no.2 Lisboa abr. 2019
https://doi.org/10.1159/000488604
IMAGES IN GASTROENTEROLOGY AND HEPATOLOGY
Baffling Cause of Upper Gastrointestinal Bleeding!
Causa desconcertante de hemorragia digestiva alta!
Amit Soni, Nirmaljeet Singh Malhi
Department of Gastroenterology and Liver Disease, SPS Hospital, Ludhiana, India
* Corresponding author.
Keywords: Gastrointestinal bleeding, Isolated gastric varices, Nonvariceal bleeding
Palavras-Chave: Hemorragia digestiva, Varizes gástricas isoladas, Hemorragia não varicosa
A 53-year-old man presented to the emergency department with recurrent bouts of hematemesis for 2 days. This was associated with dizziness and passage of black tarry stools for 1 day. He did not report any past history of a similar complaint. He denied any recent intake of NSAIDs or chronic alcohol abuse. He was living a healthy life with no comorbidity.
On examination, he had tachycardia and pallor. His systolic blood pressure was 100 mm Hg and there was evidence of postural hypotension. There was no sign suggestive of liver disease (spider angioma, decreased body hairs, etc.). Per abdomen examination was unremarkable. His initial blood tests were as follows: hemoglobin 6 g/dL; white blood cell count 7.4 × 109/L; platelets 344 × 109/L; total bilirubin 21.3 µmol/L; SGOT 33 IU/L; SGPT 27 IU/L; serum albumin 40 g/L; and INR 1.0.
The patient was transfused 3 units of packed red blood cells. After hemodynamic stabilization, an upper gastrointestinal (GI) endoscopy was done. Upper GI endoscopy revealed active spurting of blood from a vascular lesion in the gastric fundus. Endoscopically, it appeared as isolated gastric varices, so glue was injected (Fig. 1). His bleeding was controlled with glue injection.
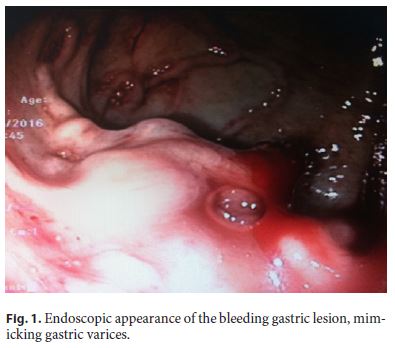
The patient was further evaluated to look for the cause of gastric varices. Color Doppler of the portal venous system was unremarkable. Computed tomographic angiography of the abdomen revealed an arterial plexus crowded in the gastric fundus (arrow in Fig. 2). It was seen to be supplied by the left inferior phrenic artery and a distal splenic artery branch (Fig. 3). The bleeding lesion which mimicked isolated gastric varices on endoscopy was actually an abnormal arterial plexus in the gastric fundus, most probably a congenital abnormality. Glue was used to plug the bleeding punctum but in view of an arterial lesion (pressure is more than a venous lesion) and a large area protruding into the stomach, chances of repeat massive bleeding were anticipated. He was referred to the interventional radiology department where embolization of the arterial plexus was done.


This case presents a rare cause of GI bleeding; i.e., an abnormal arterial plexus in the gastric fundus, likely of congenital origin. Even a Dieulafoy-like lesion could be a rare form of presentation of such a plexus. Computed tomographic angiography of the abdomen clinched the diagnosis. The lesion which appeared as gastric varix was confirmed to be an abnormal arterial plexus formed by a branch of the left inferior phrenic artery and splenic artery. Embolization of the arterial plexus remains the mainstay of treatment as this therapeutic option eradicates the plexus and hence the chances of recurrence in future. The dissociation between endoscopic and computed tomographic findings makes this case interesting and challenging.
The differential diagnosis in such cases includes isolated gastric varices, atypical Dieulafoy-like lesion, abnormal vessel coursing through the gastric wall (e.g., accessory splenic artery), and rupture of splenic artery aneurysm into the stomach [1–3]. The causes of upper GI bleeding are classified into variceal and nonvariceal causes. The need for differentiation between the two needs to be emphasized as the management varies.
Kervancioglu et al. [2] described a similar presentation of massive GI bleeding where the accessory splenic artery was the culprit and it mimicked isolated gastric varices. Authors managed the patient with coil embolization of the artery. Pinto-Marques et al. [3] described a rare case of splenic artery aneurysm which eroded into the gastric wall and presented with massive upper GI bleeding. Here we report the first case of upper GI bleeding due to an abnormal arterial plexus in the gastric wall.
References
1 Pohle T, Helleberg M, Menzel J, et al: An extraordinary Dieulafoy’s lesion presenting as varices of the gastric fundus. Gastrointest Endosc 2001;54:776–779.
2 Kervancioglu S, Yilmaz FG, Gulsen M, Kervancioglu P, Kervancioglu R: Massive upper gastrointestinal bleeding from an accessory splenic artery mimicking isolated gastric varices. Folia Morphol (Warsz) 2013;72:366–370. [ Links ]
3 Pinto-Marques P, Gíria J, Brito M, Camacho R, Loureiro R: Unusual cause for upper GI bleeding: a splenic artery aneurysm mimicking a Dieulafoy lesion. Role for systematic EUS assessment? Gastrointest Endosc 2010;71:845–846. [ Links ]
Disclosure Statement
The authors have no conflicts of interest to declare.
* Corresponding author.
Dr. Nirmaljeet Singh Malhi
Department of Gastroenterology and Liver Disease
SPS Hospital
Ludhiana, 141003 (India)
E-Mail drnjsmalhi@gmail.com
Received: November 26, 2017; Accepted after revision: March 5, 2018














