We present a case of a 65-year-old female patient, diagnosed with adenocarcinoma of the pancreatic head with liver metastasis. She underwent ERCP for biliary drainage using an uncovered self-expandable metal stent (SEMS; 6 cm × 10 mm, WallFlexTM Biliary RX Uncovered, Boston Scientific, Marlborough, MA, USA), followed by palliative chemotherapy. Eighteen months after the first procedure the patient presented to the emergency department where she was diagnosed with cholangitis and was admitted with IV antibiotics. A second ERCP was scheduled where the sphincterotome was easily introduced within the biliary metal stent but due to tumor ingrowth and overgrowth the guidewire (0.035 in × 450 cm, JagwireTM, Boston Scientific, Marlborough, MA, USA) could not transverse the stenosis, despite multiple attempts, and there was no contrast passage through stent’s proximal end (Fig. 1).
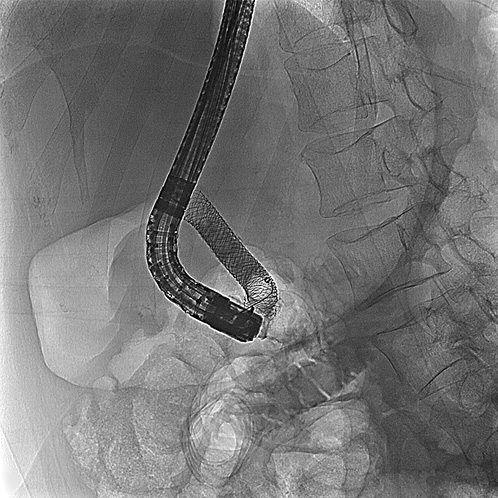
Fig. 1 Occlusion cholangiogram showing no contrast passage through the proximal end of the previously placed uncovered metal stent.
We then decided to try to achieve deep biliary cannulation using the rendezvous technique. A linear Pentax EG38-J10UT echoendoscope (Pentax medical, Tokyo, Japan) with Hitachi-Aloka HI VISION Noblus processor was used to identify the best biliary access, which was found to be transgastric. Color Doppler helped distinguish blood vessels from the dilated left intrahepatic biliary duct (Fig. 2a). A 3-mm-diameter hepatic duct was punctured by a 19-gauge fine needle aspiration needle (ExpectTM 19-gauge flex, Boston Scientific, Marlborough, MA, USA), followed by bile aspiration, confirming the correct intraductal positioning. Cholangiography was performed by injection of contrast medium through the needle (Fig. 2b). Afterwards, a guidewire was introduced in an anterograde fashion and passed all the way across the papilla into the duodenum (Fig. 3a). The echoendoscope was then removed and the guidewire tip was retrieved using a rat-tooth grasping forceps (Fig. 3b). Next a TJF-Q180V duodenoscope (Olympus Corporation, Tokyo, Japan) was introduced through the wire until the distal end of the previously placed SEMS was reached (Fig. 3c). A new SEMS (6 cm × 10 mm, WallFlexTM Biliary RX Uncovered, Boston Scientific, Marlborough, MA, USA) was deployed using the “stent-in-stent” technique (Fig. 3d), providing adequate biliary drainage. The patient was discharged the next day.
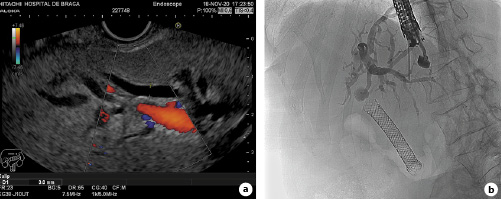
Fig. 2 - a) Endoscopic ultrasound with color Doppler showing a dilated left intrahepatic duct. b) Cholangiography after contrast injection through the fine needle aspiration needle.
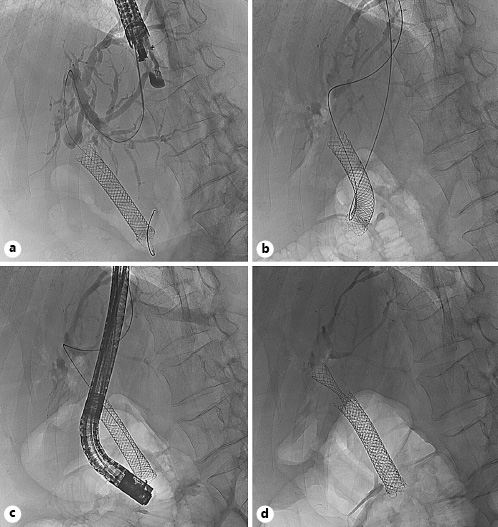
Fig. 3 A) Fluoroscopic image showing the guidewire crossing the papilla after anterograde introduction. B) Retrieval of the guidewire tip. C) Duodenoscope adjacent to the metal stent after over-the-wire introduction. d Deployment of the uncovered self-expandable metal stent using the “stent-in-stent” technique.
There are several options available when conventional deep biliary cannulation fails [1]. In this specific case, a slightly different problem arose, which was the inability to pass the guidewire through the biliary stenosis. Frequent strategies to overcome this problem consist in changing the guidewire, using a fully hydrophilic or an angled tip. Additionally, cholangioscopy could have been performed to assist the insertion of the guidewire [2], although availability and costs are important issues to consider. Finally, the fact that there was already a metal stent in situ hindered the employment of a duodenal approach for EUS-guided biliary drainage. Rendezvous procedure has been described as a salvage technique, reporting success rates around 74-80% and complication rates between 11 and 15% [3, 4]. Although it requires an experienced therapeutic ultrasonographer, EUS-guided biliary drainage has the advantage of allowing a single-operator, one-stage procedure, when compared to percutaneous transhepatic cholangiography-assisted rendezvous [5].















