Pre-endoscopy empirical PPI usage has become standard in many countries, albeit there are significant concerns in terms of masking relevant endoscopy findings, which may, among others, include eosinophilic esophagitis (EoE), thus clearly calling for a change in practice pattern [1, 2]. A 28-year-old male patient with birch pollen allergy and dysphagia for solids and reflux-like symptoms for several months with incomplete re-sponse to proton pump inhibitors (PPIs) was referred for endoscopic stricture treatment due to a presumed reflux-related stricture. Outside office-based index esophagogastroduodenoscopy (EGD), while on empiric standard-dose PPI treatment, indicated a small hiatal hernia along with a discrete short stricture. At the time, biopsies from the distal esophagus remained non-contributory.
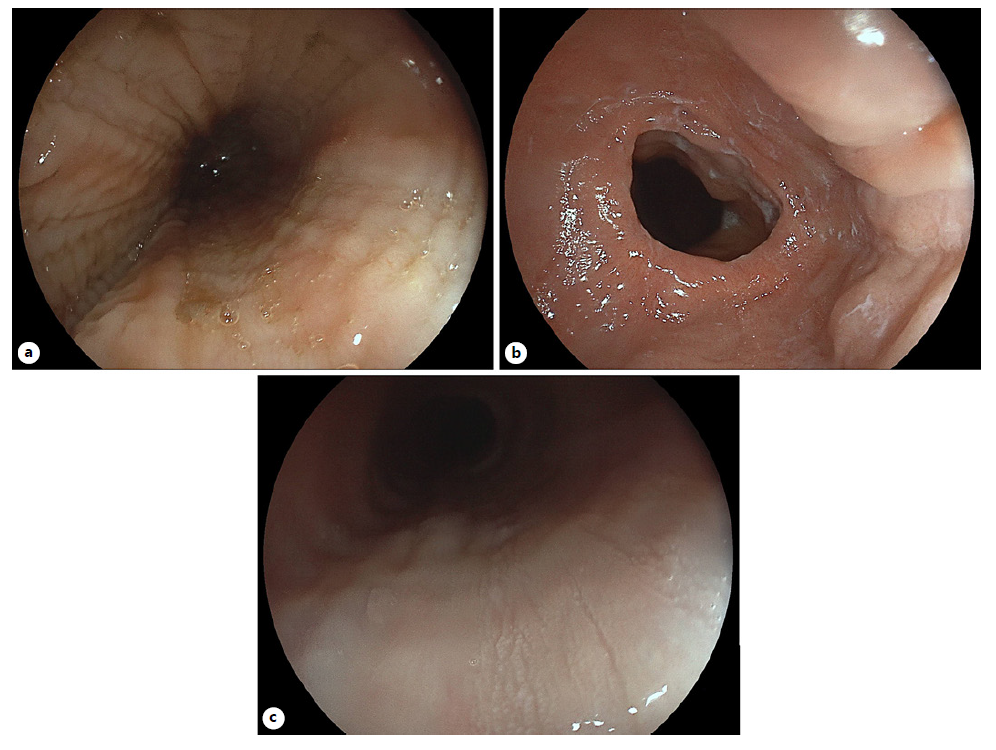
The recent EGD indicated questionable linear furrows with minor reduction in submucosal vessel visibility in the proximal esophagus (Fig. 1a). The short distal stricture was well reproduced (Fig. 1b), and a bougienage up to 20 mm using Savary-Gilliard bougies was performed (Fig. 1c; note fully preserved vascular markings in the distal esophagus). Given the lack of relevant mucosal tears after maximal bougienage (Fig. 1d), an additional radial electroincision using an IT knife was conducted (not shown). Esophageal biopsies with an adequate biopsy protocol (> two heights, >6 biopsies) yielded no evidence for potentially underlying EoE. Since the patient only benefitted transiently from the procedure and presented again after only 2 weeks with reflux-like symptoms and dysphagia, ancillary esophageal manometry did not demonstrate dysmotility. The patient consented to withdraw PPI treatment for 2 weeks with alginate bridging, causing significant clinical deterioration, i.e. worsening reflux and dysphagia. Repeat EGD provided clear-cut endoscopic EoE evidence with diffuse furrowing, diffuse lack of submucosal vessels reflecting significant edema (Fig. 2a) as well as recurrence of the distal stricture (Fig. 2b). In addition, coarse exudates were noted at the level of linear furrows, which were specifically targeted for histopathology [3, 4] (Fig. 2c - EREFS score 5). Repeat biopsies off PPI confirmed presence of EoE in this patient with a maximum infiltration of >32/HPF in the proximal esophagus. The patient was successfully treated by 2 × 1 mg orodispersible budesonide.
Empiric PPI treatment is oftentimes implemented prior to diagnostic EGD in clinical practice [5]. Unlike PPI-responsive EoE, this case of a patient falling behind endoscopic and/or pathology appreciation of EoE, while remaining highly symptomatic, should remind us to critically reconsider such practice, given that not only EoE may become masked. Beyond the need to strictly ad-here to biopsy protocol recommendations even in patients without clear endoscopic EoE stigmata, this unique clinical report illustrates the potential divergence between clinical and endoscopic response in EoE.
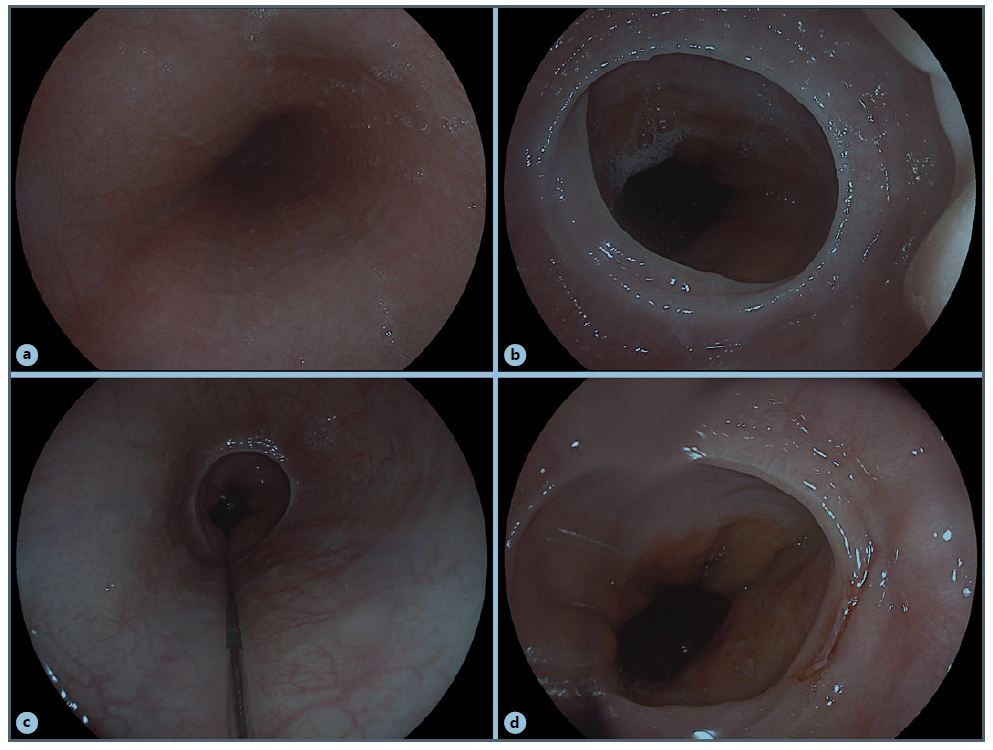
Fig. 1. a Discrete linear furrows with moderately reduced vascular markings restricted to the upper third of the esophagus. b Short distal esophageal stricture and small hiatal hernia. c Guidewire in situ prior to maximum bougienage to 20 mm; note fully preserved submucosal vessels in the distal esophagus. d Endoscopy after bougienage to 20 mm with only a minor tear at 4 o’clock.
.